
Every aspect of the Schaeffer Center’s work drives innovation. Our scholars ceaselessly explore cutting-edge ways to maximize the value of healthcare while also enhancing affordability to expand its reach.
The spread of COVID-19 over this past year served as a reminder of how vital this research truly is, as we developed viable strategies for testing as well as distribution for that moment when vaccines were ready. Indeed, amid unprecedented challenges, the record-breaking development of vaccines was a bright spot reflecting the true value and wonders of innovation.
For more than 10 years, Schaeffer Center experts have worked to advance innovative prescription drug payment models that lead to better health and long-term returns. We have shed light on the broken—and at times distorted—pharmaceutical distribution system and provided policy solutions that benefit patients. Our analyses helped spur federal regulations and state laws to save patients from spiraling out-of-pocket costs and improve access to breakthrough therapies.
Below highlights just a few studies that have made an impact over the past year. Our work informs policymakers and private-sector leaders and has been cited by the White House and Congress as well as by state and international authorities.
We continue to push new frontiers in health policy advancements by consistently introducing innovative concepts and methods to the health policy conversation. From promoting better treatments and preventive measures for Alzheimer’s to increasing the convenience of kidney care, our efforts strive to help people lead healthier lives as well as longer ones. Our research makes a real impact on improving the health of individuals and society as a whole.
Explore Schaeffer Center Research ↓

- The life sciences are at the front lines of transforming healthcare through innovations that benefit countless people. The Value of Life Sciences Innovation (VLSI) program exemplifies the Schaeffer Center’s focus on evidence-based analyses that encourage biomedical advances while developing pricing and reimbursement strategies to help ensure that patients receive the therapies they need.
-
The Schaeffer Center’s VLSI program advances strategies for spurring innovation while ensuring access.
The many successful COVID-19 vaccines and therapies developed at unprecedented speed during the pandemic provide a stunning illustration of the benefits of a robust scientific discovery system supported by investment, incentives and policy. Yet such benefits are not unique to the COVID experience. From cancer treatments and HIV/AIDS therapies to hepatitis C cures and interventional cardiology, innovations in the life sciences over the past half century have lengthened life spans by curing many deadly diseases and transforming others into manageable chronic conditions.
Still, prices remain controversial—especially in the United States, where they are generally higher than in nations that impose price controls. However, Schaeffer Center research shows that instituting price controls here would harm health in the long run. For example, as Congress considered H.R. 3, the Lower Drug Costs Now Act, Schaeffer Center modeling showed that while lower U.S. prices might improve health by increasing access in the short run, they would also hamper innovation and ultimately reduce life expectancy by about 3%. Other countries would also feel this loss, as they benefit from having Americans shoulder much of the expense of innovation.
VLSI Executive Director Karen Van Nuys, Schaeffer Center Director Dana Goldman and others at the Center have proposed value–based pricing schemes as an alternative to price controls. Such strategies link a drug’s expense to its benefits as shown in clinical trials and other data-driven methods.
One perceived roadblock to implementing value-based prices was Medicaid’s best-price rule. However, Schaeffer Center Director of Research Darius Lakdawalla and colleagues have found that, while the rule does present challenges, it need not impede progress.
Spurred by such analysis, the Centers for Medicare & Medicaid Services finalized regulatory changes allowing states, private payers and manufacturers more flexibility in value-based pricing arrangements for prescription drugs.
VLSI investigates what drives adoption patterns for biosimilar drugs.
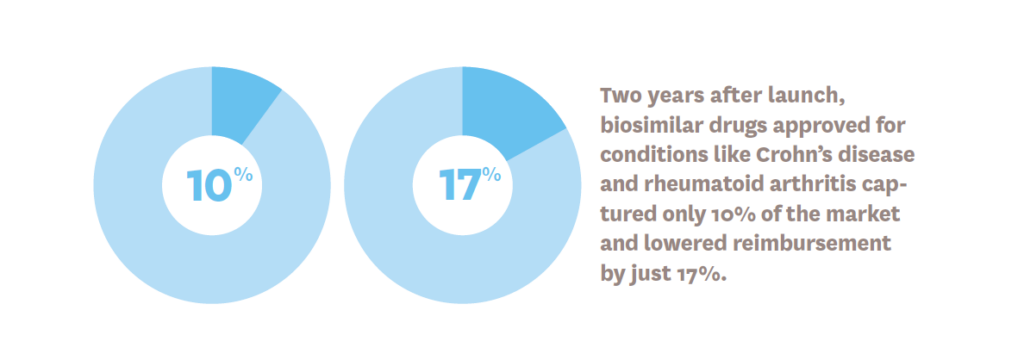
Offering the same effectiveness as biologic medications, biosimilar drugs can save money for patients and payers, but the biosimilar market has been slower to bloom in the U.S. than in Europe. Van Nuys and Schaeffer Center Senior Fellow Alice Chen have investigated the dynamics underlying this slow uptake. Their research suggests that the market is functioning but that increasing physician awareness and removing reimbursement-related barriers to biosimilar adoption can strengthen it.
“There has been some concern that U.S. biologic markets are developing too slowly, with some even arguing it’s time to give up on biosimilars and instead have the government regulate biologic drug prices outright,” Van Nuys says. “We’re not ready to give up on competition just yet—we need to understand the barriers that may be slowing biosimilar uptake, and whether alleviating them could lower costs.”
Studies reveal the relationship between higher rebates and higher prices—suggesting that eliminating Medicare’s safe harbor can save money for patients.
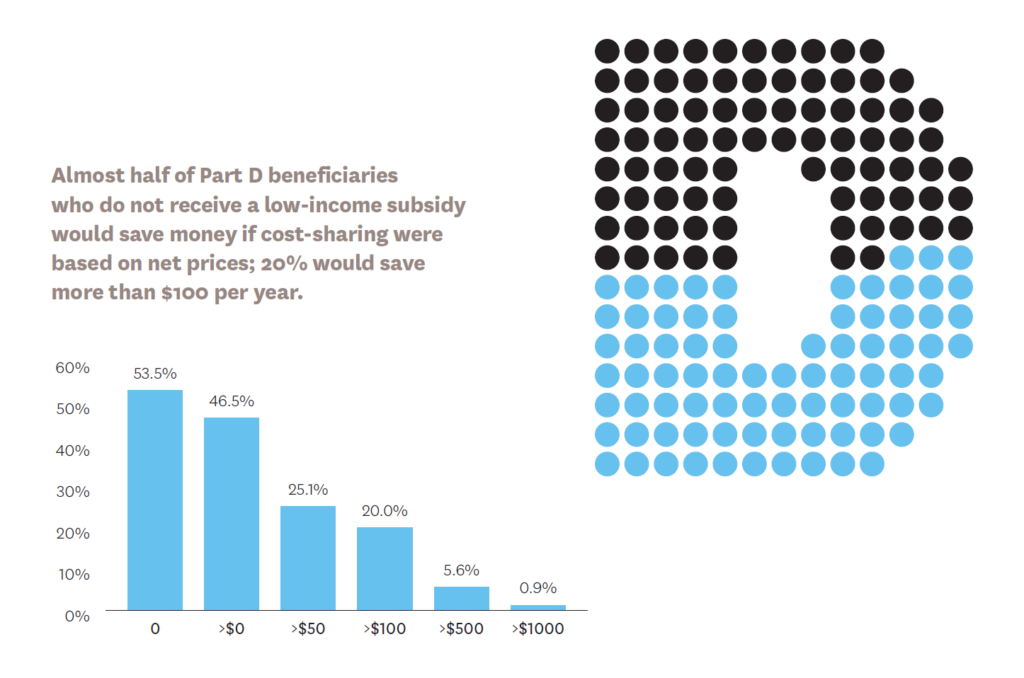
Although drug rebates are meant to save money, Schaeffer Center research suggests the opposite may be true. Since a rebate is really a kickback allowed by federal safe-harbor regulations, the current system of negotiation between pharmacy-benefits managers and manufacturers may increase prices.
Van Nuys and Schaeffer Center Senior Fellow Neeraj Sood showed that, on average, a $1 increase in rebates is associated with a $1.17 increase in list price. In addition, Schaeffer Center Associate Director Erin Trish and Director of Health Policy Geoffrey Joyce found that if Medicare cost-sharing were based on post-rebate prices, out-of-pocket spending would be reduced for nearly half of Part D beneficiaries who do not receive low-income subsidies. Some 20% of them would save more than $100 per year and about 1% would save more than $1,000 annually.
To allay concerns that eliminating the safe harbor for rebates would raise Part D premiums, Goldman and Trish showed that any premium increases would be modest, and most beneficiaries would be protected.
This evidence motivated an executive order to eliminate hidden rebates in Medicare Part D.
The Schaeffer Center explores the unique role and requirements for health technology assessment in U.S. healthcare markets.
In collaboration with the Aspen Institute, the Schaeffer Center formed an expert advisory panel to examine the U.S. healthcare system’s unique requirements and how health technology assessment (HTA) could be designed and applied here to better link the cost of innovations to their value for patients. As opposed to other developed nations, the U.S. relies almost exclusively on privately funded HTAs, but the panel sees room for public-sector funding to improve our country’s disjointed approach.
The panel proposes six recommendations that, taken together, would enhance the HTA landscape and improve decision making:
- Encourage private HTA efforts
- Establish a publicly funded HTA coordinating entity to augment private efforts and evaluate their overall quality
- Ensure that HTA reports present clinical and economic findings in a disaggregated format
- Evaluate existing and new healthcare services and technologies, including drugs, devices, diagnostics, procedures and public health interventions
- Engage healthcare providers, consumer groups, public and private payers, employers and the life sciences industry in the activities of any public HTA entity
- Create a policy path for the HTA coordinating entity’s findings to influence decisions
“The U.S. market fails to produce enough high-quality evidence,” says Lakdawalla, who co-chaired the panel. “Robust, unbiased assessments of the evidence can help accelerate the long overdue transition to value-based pricing in healthcare.”

- Behavioral science combines insights from psychology, economics and other social sciences to understand how people make decisions relevant to their wellbeing. The Schaeffer Center applies the field’s knowledge to find ways to enhance that wellbeing. This research took on increased urgency as COVID-19 began proliferating throughout the world.
-
During a tumultuous year, Schaeffer Center investigators applied methods from behavioral science to better understand individual responses to safety measures and election polling.
As COVID-19 rapidly unfolded in spring 2020, health leaders urged behavioral changes— including social distancing—to contain its spread. Although many followed these guidelines, others flouted them.
To understand how and why Americans responded in those crucial early days, Wändi Bruine de Bruin—co-director of the Behavioral Sciences program—and colleagues polled 5,414 nationally representative adults through the online Understanding America Study. The study showed that those perceiving greater danger—partly based on case numbers locally and nationally as well as age and economic factors—were more likely to implement protective behaviors. These findings could help leaders improve communication and implementation of mitigation strategies as we continue to battle COVID-19—and better prepare for future pandemics.
Meanwhile, Bruine de Bruin used politics as a lens to analyze the flaws in standard polling. For example, traditional polls ask people whom they would vote for if an election were held today or their likelihood of voting for specific candidates. But Bruine de Bruin found that asking people about the political preferences of those in their social circles and in their states could paint a more complete picture of the American electorate.
“People often get information about political issues from friends and family—and those conversations may influence their voting choices,” Bruine de Bruin and her co-authors note.
The USC Behavioral Science and Well-Being Policy Collaboration unites experts from across disciplines to promote policies with positive social impact.
Because behavioral science is by nature multidisciplinary, its leading minds are spread across a range of departments at a variety of institutions. This new collaboration, led by Bruine de Bruin and Jason Doctor—director of health informatics at the Schaeffer Center and co-director of the Behavioral Sciences program— is building a network of communication and research partnerships among these experts through conferences, seminars, a website and co-authored studies.
The collaboration’s activities will strengthen research in subjects from personal finance and poverty to climate change, environmental risks and security—all of which affect human health.
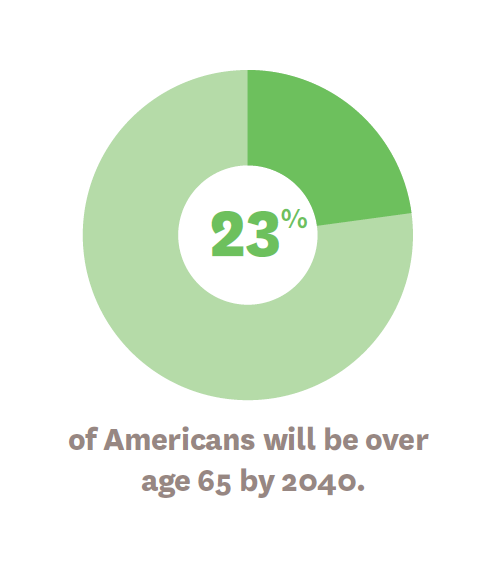
Twenty years from now, adults age 65+ will make up more than 20% of the U.S. population—and physicians and health systems will need guidance to support their efforts to provide them with the best care.
The new USC Roybal Center for Behavioral Interventions in Aging was created to strengthen the ability of clinicians to recommend safe and effective treatments for elderly patients through evidence-based behavioral economic interventions.
With funding from the National Institutes of Health, the center’s co-principal investigators—Schaeffer Center Director Dana Goldman and Jason Doctor, Director of Health Informatics—lead research that advances healthy aging for older adults, with a focus on those who are economically insecure, culturally diverse and underserved by human services organizations. The center’s studies include stemming the opioid crisis by influencing physicians to avoid unnecessary prescriptions.
BMJ published a study co-authored by Doctor and Schaeffer Center Fellow Daniella Meeker that builds on their groundbreaking work in low-cost nudges that improve prescribing practices. To help ensure the success of such interventions, the authors suggest that:
- nudges should be carefully designed and implemented for awareness and ease of use by clinicians.
- details such as orienting clinicians to goals and publicizing their commitment are important to success.
- strategies should be adjusted to address the needs of different groups and clinical contexts.
- trust between clinicians and administrators is critical.
The nudges devised by Doctor and colleagues are being increasingly adopted across the nation as well as in the United Kingdom.

- COVID-19 has cost millions of lives worldwide, overwhelmed healthcare systems, devastated economies and changed society for years to come. To ease the pandemic’s impact, the Schaeffer Center immediately launched research to improve public safety while getting people back to work without fear of infection.
-
The Schaeffer Center is partnering with the city of Los Angeles to examine the advantages of rapid antigen testing to track COVID-19 and reopen schools and businesses safely.
Schaeffer Center Senior Fellow and Director of the COVID Initiative Neeraj Sood is collaborating with the Los Angeles County Department of Public Health and the Los Angeles Mayor’s Office to examine the advantages of rapid antigen testing among first responders and school-aged children. Rapid tests have the potential to quickly alert people who are contagious and need to isolate, thereby stopping the chain of transmission.
The study examines antigens—which trigger our immune systems to produce virus fighting antibodies—in the bloodstream of both symptomatic and asymptomatic participants to understand how COVID-19 spreads in different communities. The pilot study may help determine the best ways of leveraging these inexpensive tests to facilitate safe reopening efforts. Los Angeles is one of the nation’s first metropolitan areas to launch a large-scale study of rapid tests in both symptomatic and asymptomatic participants.
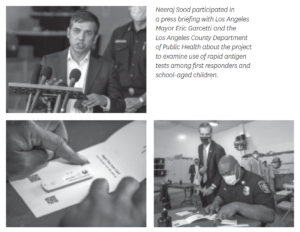
Mayor Eric Garcetti held a press conference in October 2020 with Sood to discuss the project. “Rapid tests are cheaper, faster and more accessible—and they are a potential game-changer in our ability to respond to COVID-19, reopen our schools and get our economy back on track,” Garcetti told journalists. “Los Angeles never shies away from a challenge, and we are tapping into our trademark creativity, our innovative spirit, and our strong partners with USC and the county to advance groundbreaking research, prevent the spread of this virus and save lives.”
The second phase of the project seeks to assess the feasibility, acceptability and accuracy of repeat rapid antigen testing for screening school-aged children. The researchers hope to establish the best way to deploy rapid testing, how often each student should be tested and the most efficient large-scale testing methods.
Rapid and effective vaccine distribution requires a well-designed plan. Schaeffer Center fellows explored ways to build the infrastructure to facilitate quick and effective vaccination.
Even the most potent vaccine only works if it reaches communities quickly. The Schaeffer Center leveraged scientific and strategic expertise to help local, state and federal governments make the difficult decisions crucial to efficient distribution.
Schaeffer Center Senior Fellow Jeffrey McCombs and colleagues emphasized the importance of community pharmacists to any immunization effort. “Roughly 9 out of 10 Americans live within five miles of a pharmacy with the capacity to provide vaccinations during extended hours and without an appointment,” they wrote. However, to be truly effective, “state practice laws concerning vaccine prescribing authority should be uniform across states and written to automatically include new vaccines once they are approved by the Food and Drug Administration.”
In February 2020, Schaeffer Center Director of Health Policy Geoffrey Joyce brought attention to the dangers of shortages posed by supply chains. In an interview with the Los Angeles Times, he said, “the vast majority of raw materials that go into a prescription drug are produced overseas, mostly in China and India.” As a result, he noted, “[t]he coronavirus shutting down China or India for an extended period of time is likely to have a substantial impact on the supply of many drugs.”
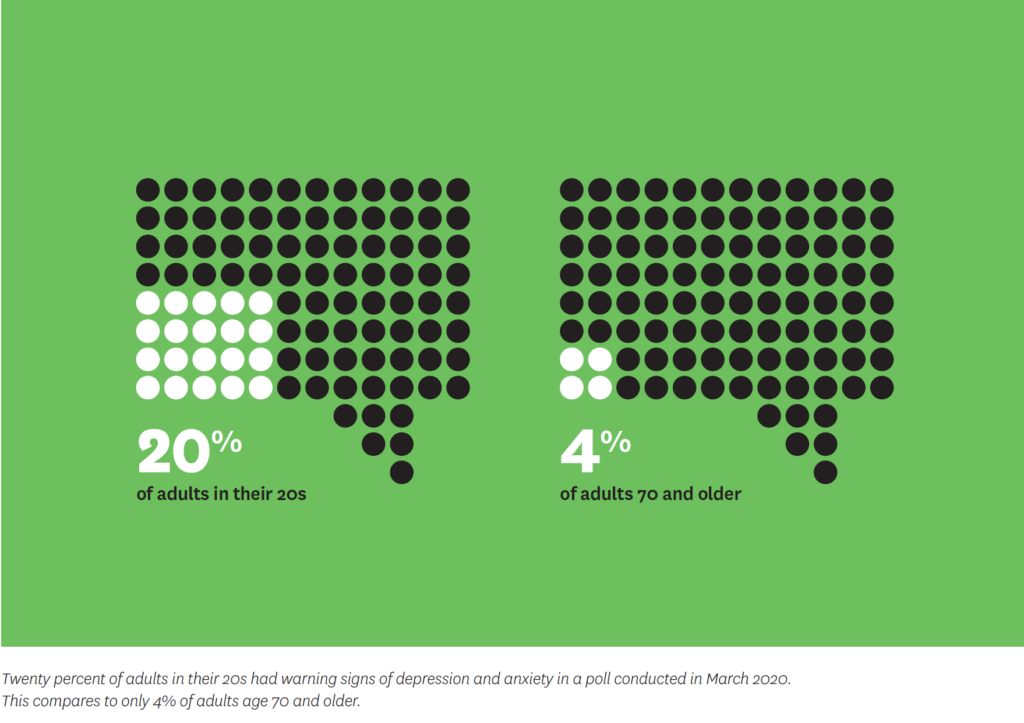
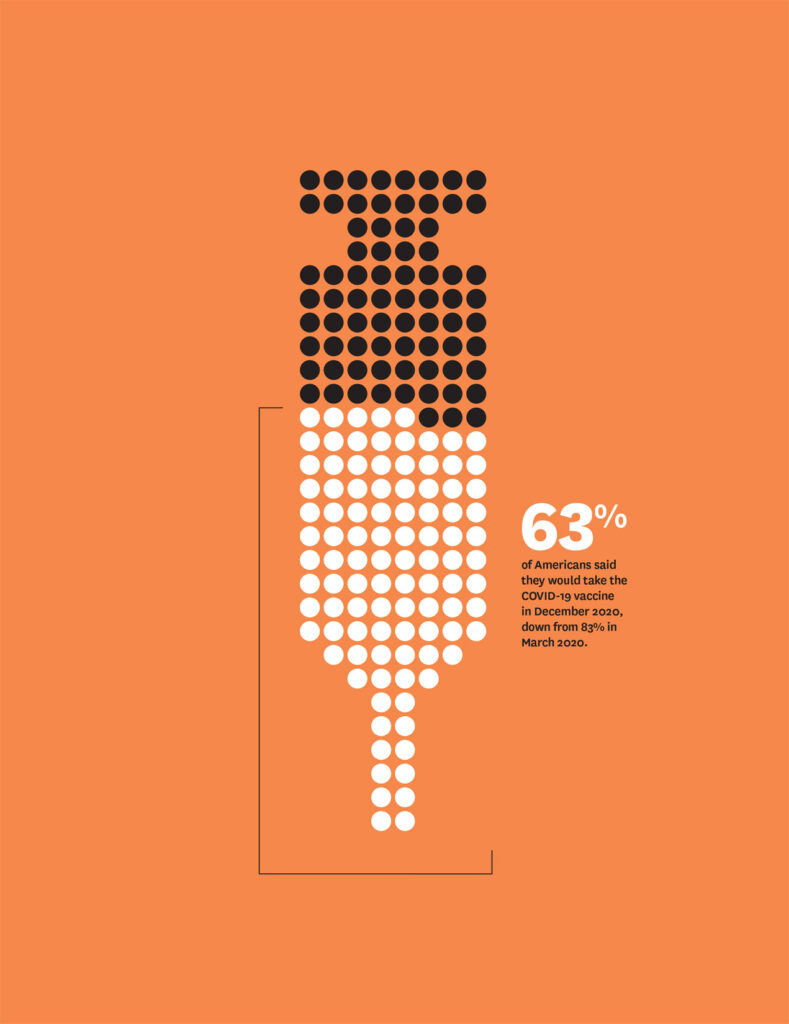
In addition, vaccine hesitancy is a major concern. According to a survey of Americans conducted in December 2020, only 63% said they would take the COVID-19 vaccine, down from 83% in March 2020. “These results suggest that we need to have good strategies in place very soon to ensure the greatest possible uptake of vaccines,” said Wändi Bruine de Bruin, co-director of the Schaeffer Center’s Behavioral Sciences program, during an expert panel on vaccine adoption hosted virtually by the Schaeffer Center.
Schaeffer Center Director Dana Goldman, Senior Fellow John Romley and Visiting Scholar Matthew A. Crane examined the public health challenge of vaccine hesitancy and urged transparency from public health agencies at all levels to address safety concerns. Communication with minorities, especially the Black community, is especially vital as they may be distrustful of vaccines due to historical wrongs.
Analysis promotes widescale random testing and greater care with personal protective equipment.
In March 2020, Sood penned an opinion piece in The Wall Street Journal calling for random testing rather than only testing the symptomatic to better understand community spread. Schaeffer Center Fellow William Padula expanded on this idea. Writing in Applied Health Economics and Health Policy, Padula noted “there is substantial evidence to support the belief that many of the infected population are asymptomatic.” Therefore, “the U.S. should consider randomizing testing in the general population.”
Padula also found that long hours of wearing the same mask may result in facial injuries, rendering caregivers vulnerable to the very virus from which the gear aims to protect them. “Healthcare facilities should establish clear policies for educating frontline staff on steps to maintain personal hygiene and protect the health of vulnerable, noninfected patients in addition to those presenting with COVID-19,” he and colleagues wrote in a position paper for the National Pressure Injury Advisory Panel.
As COVID-19 began spreading, so did disagreements about its hazards and how to respond. Schaeffer Center research emphasized the importance of clear messaging and public alerts to protect people from COVID-19.
Bruine de Bruin conducted a national study that highlighted the importance of clearly communicating the disease’s risks. She found that people who understood the potential dangers were more likely to take protective measures.
“Unless addressed by effective health communication that reaches individuals across all social strata, variations in perceptions about the COVID-19 epidemic raise concerns about the ability of the U.S. to implement and sustain the widespread and restrictive policies that are required to curtail the pandemic,” Bruine de Bruin and her fellow researchers wrote.
In a co-authored op-ed for the Los Angeles Times in April 2020, Goldman proposed modifying California’s smog alert system to warn people of COVID-19 spikes. Such “virus alerts” would be triggered by high levels of infection or mortality rates.
“People could return to work while observing reasonable safety rules, such as wearing masks in public places and practicing social distancing in restaurants and workplaces,” Goldman and his co-author wrote. To that end, they also encouraged public service campaigns reminding the public to follow these commonsense safety measures.
Schaeffer experts offer pooled testing as a cost-effective measure to help safely reopen businesses and schools.
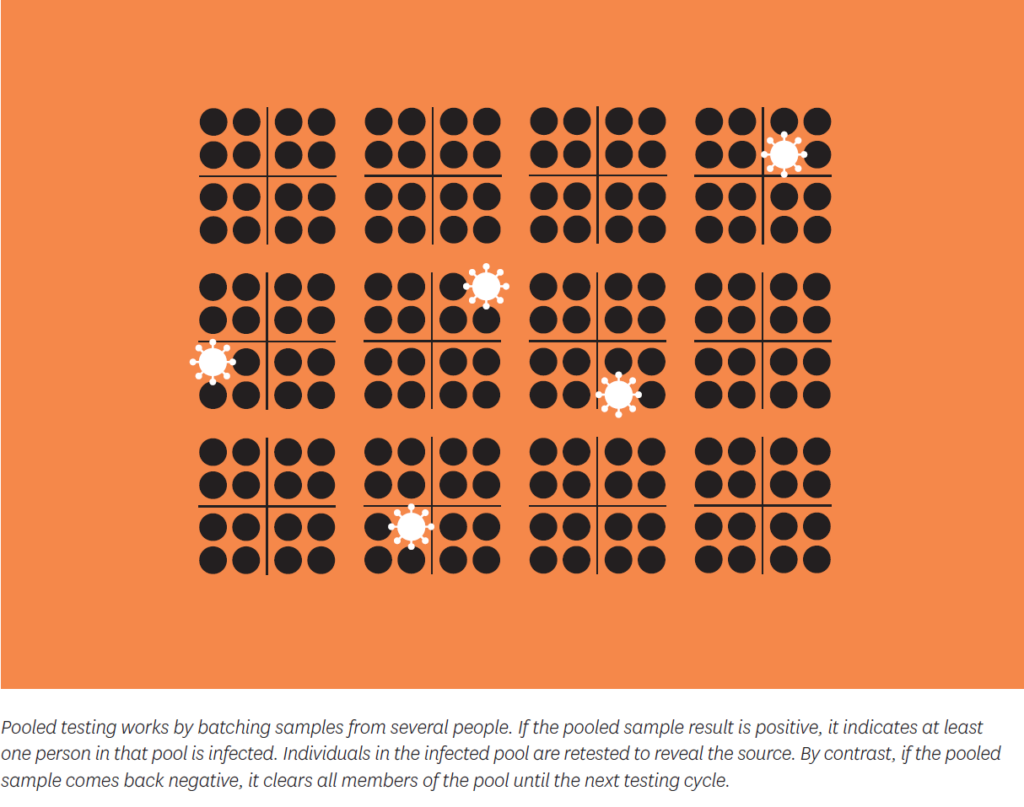
As the pandemic spread and testing supplies became more limited, screening as many people as possible as quickly as possible became urgent. In July 2020, Schaeffer Center Director of Research Darius Lakdawalla, Associate Director Erin Trish and Goldman proposed pooled testing as a way to safely reopen businesses and schools.
Instead of laboratories running tests on each individual in a company or school, pooled testing processes samples in batches. If a result shows one or more infections, individual testing is used to find the source. However, if the pool comes back negative, all members are cleared for in-person work or school.
The team found that pools of four are optimal—and would cut costs of periodic testing by more than half while providing accurate results. In response to this research, the Food and Drug Administration began issuing emergency- use authorizations for pooled-testing techniques and school administrators reached out to Schaeffer Center experts for advice. The findings also garnered nationwide media coverage.
Schaeffer Center research examined the balance between public health concerns and the economic consequences of COVID-19.
Nobel Laureate and Schaffer Center Distinguished Fellow Daniel McFadden analyzed a worst-case scenario of the pandemic in spring 2020, finding that it could cause up to 4.5 million deaths among older Americans. Fortunately, policymakers heeded enough advice from experts, including Schaeffer Center fellows, to avoid that outcome, but the toll has still been tragically high.
To avoid the worst, Mireille Jacobson, codirector of the Schaeffer Center’s Aging and Cognition program, wrote in STAT in March 2020: “We should all be prepared to make significant economic sacrifices now to minimize the harm of this evolving crisis. Furthermore, we should provide assistance to help those who are disproportionally affected by such measures weather the current storm and get back on their feet once the epidemic has passed.”
Joyce examined the economics of COVID-19 for MarketWatch in April 2020. “Some economists and business leaders believe the costs of constraining the virus have exceeded the benefits,” he wrote. “They point to unemployment totals not seen since the Depression and entire industries shut down, compared to virus death totals that may reach only the numbers from a bad flu season (55,000).” However, Joyce noted, the emerging data showed that governments had no choice but to impose restrictions. “Assuming that mortality rates would rise from 0.5% to 1.5% as hospitals become increasingly overrun, the estimated cost of COVID-19 increases to $5.6 trillion,” he calculated.
A Schaeffer Center model showed the potential value of new COVID-19 therapies—in vivid terms of lives saved and dollars conserved.

Schaeffer Center Fellows Karen Mulligan and Karen Van Nuys, along with Joyce, used a data model to consider the financial and health related benefits of two hypothetical treatments.
They estimated that an outpatient treatment reducing hospitalization risk by 50% would result in 285,000 fewer hospitalizations, up to 71,000 fewer deaths and almost $88 billion in value by the end of 2021. Meanwhile, a hospital-based treatment that reduces mortality and length of stay by 30% would save between 51,000 and 85,000 lives, generating up to $106 billion in value during that same period.
“With the U.S. not pursuing a strategy of ‘crushing the virus’ like Europe and Asia, treatment to manage the virus’s impact becomes even more valuable,” they wrote. This was especially true before vaccines became available. Yet innovative treatments will remain vital to COVID-19 management, as vaccines are not perfect and some people will refuse inoculation.
“We will need to manage COVID-19, and possibly other novel viruses, for years to come,” the team added. “A vital tool will be effective treatments. We must prioritize their development now. If we do, we will be rewarded with resilient health systems, a stronger economy and longer lives.”
The USC-Brookings Schaeffer Initiative helps consumers navigate the insurance market to get better healthcare value—with the pandemic adding new urgency.
As COVID-19 cases mounted, the Affordable Care Act (ACA) enabled many families to obtain subsidized coverage during special enrollment periods or if they had lost coverage along with a job loss. However, those who are excluded may turn to insurance that does not comply with ACA standards.
The USC-Brookings Schaeffer Initiative for Health Policy helped protect families by disseminating information on the pitfalls to avoid and the types of comprehensive coverage to look for. The initiative also explained how and where to sign up. The authors noted, however, that people had to act fast. In many cases, the deadline for getting coverage is 60 days after the previous plan ends—and healthcare costs often remain uncovered until enrollees sign up.
In a story for Marketplace in May 2020, USC-Brookings Schaeffer Initiative Fellow Christen Linke Young explained that the plans “are likely more affordable than people may be expecting,” adding that the plans are subsidized and based on estimated total yearly income. “On average, for people who bought a plan on healthcare.gov last year, the financial assistance covered 87% of the premium.”

- Alzheimer’s disease is the most common form of dementia and a leading cause of death for older Americans. It currently afflicts more than 5 million people across the country—a figure that threatens to triple in the next 40 years. But new therapies are on the way, and the Schaeffer Center is exploring options to facilitate their use, improve clinical trials, and ease the burden of the disease for patients and families.
-
With breakthroughs on the horizon, Alzheimer’s disease may finally meet its match, but health systems must be prepared.
New Alzheimer’s disease treatments and prevention strategies are drawing near, with a reported 132 drugs in the pipeline. Many of these could slow or reverse development of Alzheimer’s telltale brain plaques, called amyloids.
“We are close to major breakthroughs,” said Paul Aisen, founding director of the USC Alzheimer’s Therapeutic Research Institute, during a webinar held by the USC-Brookings Schaeffer Initiative for Health Policy. Leonard Schaeffer introduced Aisen, who noted that advances in brain imaging and blood-based biomarkers may help with Alzheimer’s prevention.
Schaeffer Center Director Dana Goldman moderated the panel, which included Sharon Cohen, medical director of the Toronto Memory Program at the University of Toronto, and Heather Snyder, vice president of Medical and Scientific Relations at the Alzheimer’s Association.
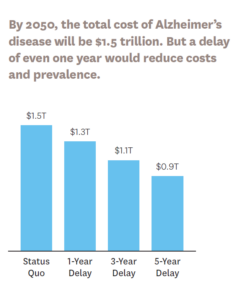
A second panel discussed possible models to pay for novel treatments. Schaeffer Center Director of Research Darius Lakdawalla suggested that USC’s Future Elderly Model microsimulation could help estimate long-term health consequences of functional and cognitive decline and associated costs, and inform a pricing strategy that would reflect the
lifetime health burden of Alzheimer’s.Early interventions are key. Citing Schaeffer Center research, panelist Sarah Lenz Lock, senior vice president for Policy and Brain Health at AARP, noted that if innovative drugs reduce the risk of getting Alzheimer’s by 20% to 40%, or can delay onset by five years, the overall cost burden could be cut in half.
However, more people need regular assessments so interventions can be employed. A Schaeffer Center study led by Aging and Cognition program Co-Director Mireille Jacobson showed that only one-fourth of Medicare patients report receiving cognitive assessments during annual wellness visits, even though they are a required component.
Schaeffer Center researchers uncover why Alzheimer’s clinical trials are slower to enroll participants, take longer to complete and are more expensive than those for other conditions. Our investigators explore strategies for long-term well-being.
In a survey of nearly 900 Alzheimer’s stakeholders, researchers found that 99% of eligible patients are never referred to or consider participating in an Alzheimer’s clinical trial. Schaeffer Center experts say that patient organizations, healthcare providers, researchers, government and industry must work together in a holistic approach to reform clinical trials for Alzheimer’s, improving awareness of the disease and facilitating participation in trials among diverse patients.
A healthy lifestyle and management of risk factors such as high blood pressure and high cholesterol could reduce dementia rates.
Certain combinations of cardiovascular drugs may reduce the risk of Alzheimer’s disease, according to a Center study of nearly 700,000 Medicare beneficiaries. Since 1 in 4 adults over age 65 uses both antihypertensives and statins, treatments already in use could reduce the number of people with Alzheimer’s and related dementias.
The Schaeffer Center is exploring new ways to ease the toll of Alzheimer’s disease on individuals, families and caregivers, along with strategies to reduce the burden on health systems.
With a $4.1 million grant from the National Institute on Aging, the Schaeffer Center launched the multisite Center for Advancing Sociodemographic and Economic Study of Alzheimer’s Disease (CeASES-ADRD). Led by Julie Zissimopoulos, co-director of the Aging and Cognition program, CeASES-ADRD confronts the enormous health, economic and social costs of Alzheimer’s disease by increasing knowledge and technological capacity and building a global network of researchers. Partners include Stanford University and the University of Texas at Austin.

- Health inequity is one of today’s most urgent challenges. The Schaeffer Center develops high-value strategies to improve the wellbeing of vulnerable and underserved populations. Our research explores issues confronting patients of all ages and backgrounds—as well as systemic issues within the healthcare system.
-
Each generation of less-educated Americans reports more pain throughout their lives than their elders, and education may hold the key.
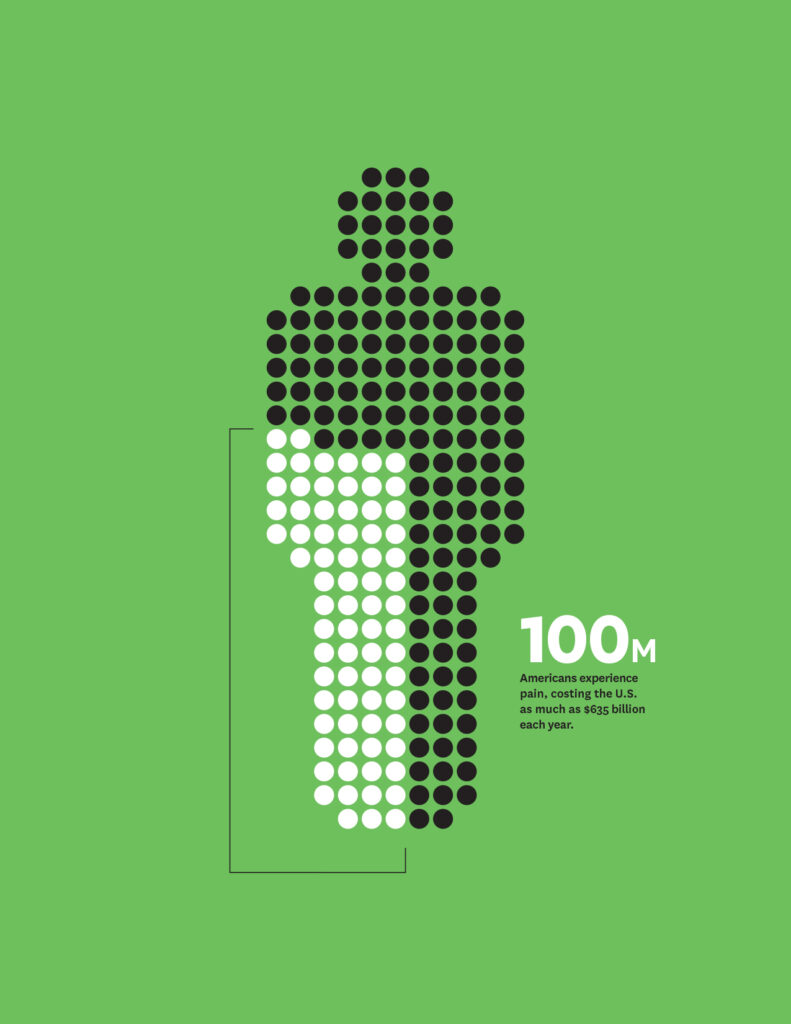
Schaeffer Center research reveals that middle-aged Americans now report more pain than the elderly, and reports of pain are rising more quickly in younger people. The trend seems to be driven by the two-thirds of U.S. adults without a four-year college degree. This troubling
finding seems to be unique to our nation— and is rising with each generation.The intergenerational increase could be driven by numerous factors to which the less educated are vulnerable—including stagnant wages, unemployment, broken homes and social isolation. If the trend continues unchecked, tomorrow’s elderly will be sicker than older people today, presenting even greater challenges for the healthcare system that tends to their needs.
In conducting the study, Nobel Laureate and Schaeffer Center Distinguished Fellow Sir Angus Deaton, Princeton Professor Anne Case and Schaeffer Center Fellow Arthur Stone drew from surveys of more than 2.5 million adults in the United States and Europe. The research builds on previous work by Deaton and Case that coined the term “deaths of despair.”
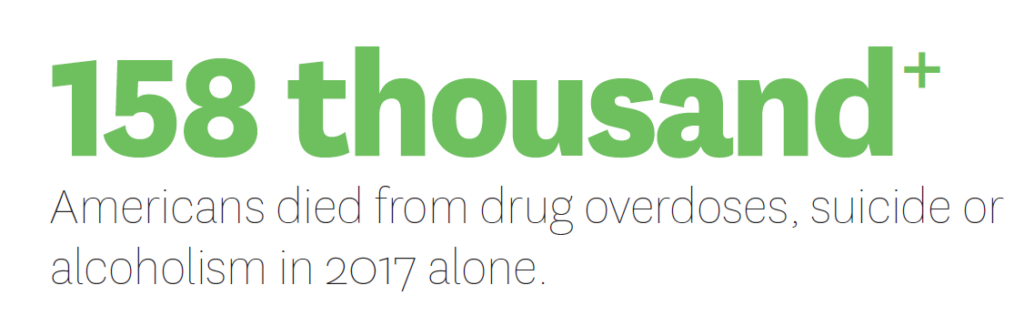
Deaton and Case’s bestselling book, Deaths of Despair and the Future of American Capitalism, documents the devastating deaths that preceded COVID-19. In 2017 alone, 158,000 Americans died from drug overdoses, suicide or alcoholism. The toll contributed to the first three-year drop in U.S. life expectancy since the flu pandemic of 1918.
Although policymakers have tried to address opioid addiction as a main cause, Deaton and Case argue that these addictions merely accelerated an already existing epidemic. Opioid overprescribing also provides a glaring example of how the U.S. medical system has failed to uphold its mandate of improving people’s health.
The Schaeffer Center promotes policies to ensure high-quality care for kidney patients.
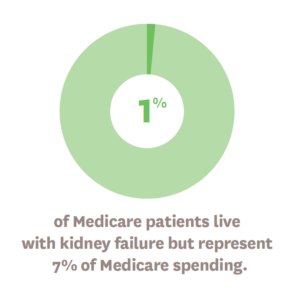
Schaeffer Center Fellow Eugene Lin and Director Paul Ginsburg co-authored an influential report on the dominance of in-center dialysis care, which has persisted despite home-based alternatives offering similar outcomes and often being preferred by patients. In 2019, a presidential executive order, Advancing American Kidney Health, was signed to enable more patients to receive dialysis treatments at home—increasing patient satisfaction while reducing Medicare costs.
A new digital initiative collects data from across sociodemographic groups to improve population health and reduce disparities.
The American Life in Real-Time project is building the first large-scale, digital health dataset that will represent everyone in the nation—including previously underrepresented ethnic and economic groups. The Schaeffer Center launched the initiative with the RAND Corporation and Evidation Health to correct the bias in most data sets that investigators rely on. For example, as information collected by internet-enabled devices is increasingly used to study public health, people who cannot afford or choose not to purchase such technology are being left out of data pools.
Schaeffer Center research examines how states are tackling the opioid crisis to promote best practices for stemming addiction.
Ten Western states reported an increase of nearly 100% in deaths caused by synthetic opioids in 2020. To promote effective tactics for stopping the tidal wave of opioid addiction, Schaeffer Center Senior Fellow Rosalie Liccardo Pacula collaborated on an examination of three approaches taken by states:
- Increasing healthcare insurance coverage and payment rates
- Expanding treatment capacity
- Developing more comprehensive and connected treatment networks
The study notes that, thanks to federal efforts and certain state initiatives, substance use treatment organizations are gradually becoming better integrated into the overall healthcare system. However, the process has been slow and mostly unknown to the public. Further, more needs to be done to modernize information systems so those helping people overcome addiction can better communicate with insurers.
Researchers calculate the lifetime costs of adult congenital heart disease.
Schaeffer Center Fellow Cynthia Gong, Health Policy Microsimulation Director Bryan Tysinger and Schaeffer Center Director Dana Goldman modeled the lifetime health, education, labor and social outcomes of people with congenital heart disease. They found that adults with the condition face a lifetime burden of $500,000 compared to those who are healthy. The study used the Future Adult Model, an economic demographic microsimulation that covers the entire U.S. population to study the lifetime impacts of chronic diseases.
A Schaeffer Center expert evaluates markets for recreational drugs to examine their health ramifications.

As more states and nations legalize marijuana for recreational use, policymakers rely on Pacula’s expertise for evidence-driven analysis of the long-term effects of decriminalization. In her role as president of the International Society for the Study of Drug Policy, Pacula has testified before the United Nations and World Health Organization and has briefed state legislatures and the Centers for Disease Control and Prevention.
Vaping represents a particular health concern, especially since young e-cigarette users have been shown to be five times more likely to be diagnosed with COVID-19 than nonusers. However, Pacula suggests that making e-cigarettes illegal would simply drive the market underground—making it harder to track health effects.
“The unregulated vaping market today is a Wild West of hucksters, unsubstantiated claims and unknown ingredients. The health of our nation, particularly our young people, is riding on getting it under control,” said Pacula, for an article that appeared in The Hill.
Who receives advanced stroke care may depend on traffic.
Schaeffer Center Fellow Sarah Axeen and colleagues at the Keck School of Medicine at USC analyzed how long it took emergency medical services to transport patients to hospitals with comprehensive stroke centers in L.A. County. The study revealed that shifting traffic conditions—not distance—result in nearly 20% of the population having only intermittent access to care. The researchers hope these findings will influence how planners and public health professionals allocate resources and think about access.

- U.S. medical costs are the highest in the world—but vast spending does not automatically result in healthier outcomes. By measuring and analyzing value in healthcare and proposing insightful and affordable ways to enhance resources, Schaeffer Center experts are helping improve healthcare for all.
-

Higher spending does not necessarily lead to better cancer outcomes— especially at the end of life.
Schaeffer Center Director of Research Darius Lakdawalla and Schaeffer Center Director Dana Goldman reviewed studies that examined the relationship between spending and outcomes in cancer in the U.S. and internationally. They found that higher cancer spending, in international comparisons, was almost always correlated with better outcomes and lower mortality. However, spending in the United States—especially when focused at the end of life—did not always produce better outcomes and was frequently associated with higher mortality.
Writing in the Journal of Clinical Oncology, the team noted that although the average patient in the United States has faster access to a greater number of innovative treatments and services, overall costs are driven up through wasteful spending. Studies of alternative care delivery and revised payment models indicated that lower spending is achievable without adversely affecting outcomes, with the best results coming from efforts to limit expensive hospital use.
The Schaeffer Center’s new Healthcare Markets Initiative explores novel ways to deliver value and improve efficiency.
U.S. healthcare markets suffer from both overuse and underuse. The challenge is how to create market incentives to eliminate the inefficiencies that make some services too expensive and many public-sector reimbursements too low. Led by Lakdawalla and Nonresident Senior Fellow Joe Grogan, the Healthcare Markets Initiative brings together experts and innovators to seek ways of redesigning healthcare markets to improve their function.

Taking a broad view of medical services, drugs, devices and insurance, the Healthcare Markets Initiative examines numerous areas for potential improvements, such as encouraging innovation to treat chronic disease, making health insurance markets work more efficiently, improving regulation to support medical innovation and designing pay-for-performance frameworks.
A Schaeffer Center study examined life-expectancy gains in recent decades for healthy Americans and those with chronic conditions such as diabetes, hypertension and coronary artery disease.
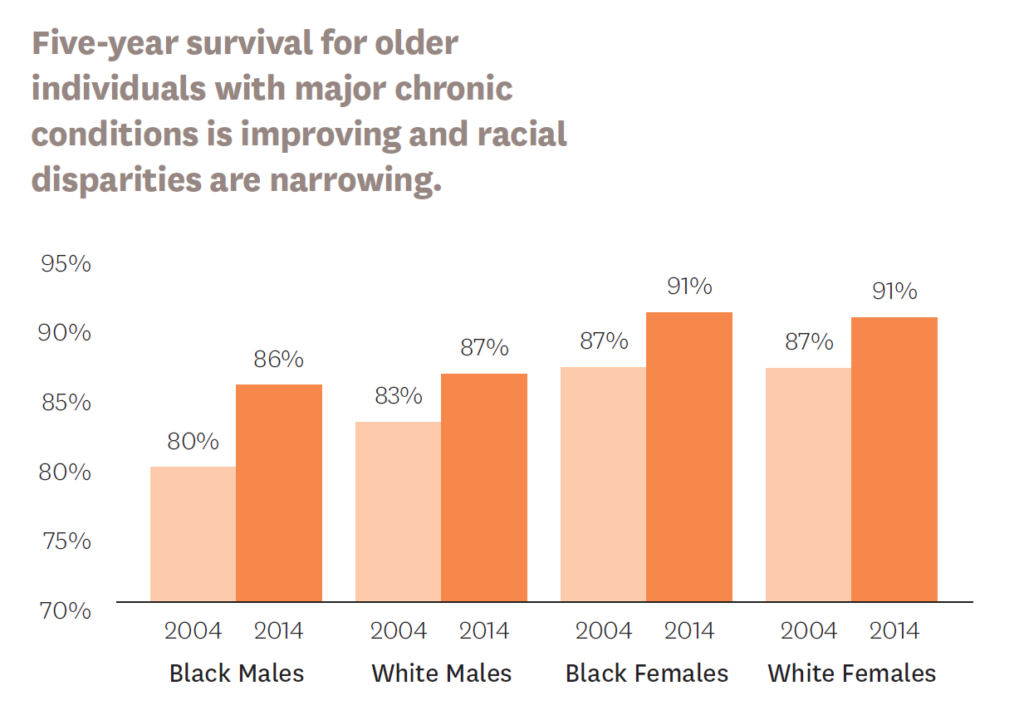
Published in Health Economics, the research found that in people with or without chronic conditions, survival gains were significant only among those over age 65—notably, the sole group in the U.S. with universal access to public insurance. Racial disparities in life expectancy also narrowed with access to Medicare.
While the U.S. has achieved significant reductions in cancer mortality, it’s been an expensive endeavor—with oncology spending rising from $27 billion in 1990 to $137 billion in 2017.
In a study published in the Journal of Policy Analysis and Management, Schaeffer Center experts explored whether cancer detection and mortality rates shifted at age 65, when Americans become eligible for Medicare.
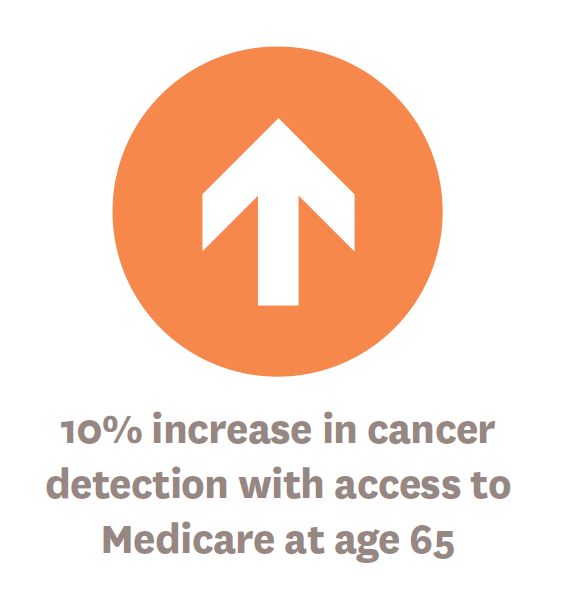
Focusing on breast, colorectal and lung cancer—since guidelines recommend screenings for those conditions before and after age 65—they found that access to Medicare coverage increased cancer detection by 10% at age 65 compared to people just one to two years younger. In terms of survival, the analysis revealed a 4.5% decrease in cancer mortality for women age 65 when contrasted with women ages 63–64—and results were even better for Black women, who saw cancer mortality drop by 9% compared to their slightly younger peers.
The authors’ conclusion: Universal coverage improves detection and outcomes, especially for underserved populations that may delay healthcare if they have inconsistent insurance coverage.

- The USC-Brookings Schaeffer Initiative for Health Policy combines the data and analytic strengths of the Schaeffer Center with the policy expertise of Economic Studies at Brookings. In the five years since its founding, the initiative has become an influential powerhouse that informs the national healthcare debate with rigorous, evidence-based
analysis and practical recommendations. -
Surprise medical billing has become one of the most pressing topics in healthcare, and USC-Brookings experts have been prolific contributors to analysis of the issue and policy solutions.
Too often after a hospital procedure or visit to an emergency room, patients get hit with unexpected bills from out-of-network providers—such as anesthesiologists, emergency room doctors and radiologists—that they had no role in choosing.
Under the leadership of Paul Ginsburg, the USC-Brookings Schaeffer Initiative for Health Policy produced seven publications on surprise billing over the past year, including investigations of different states’ laws, the most common sources of surprise bills and how policies to address surprise billing could lower premiums for all.
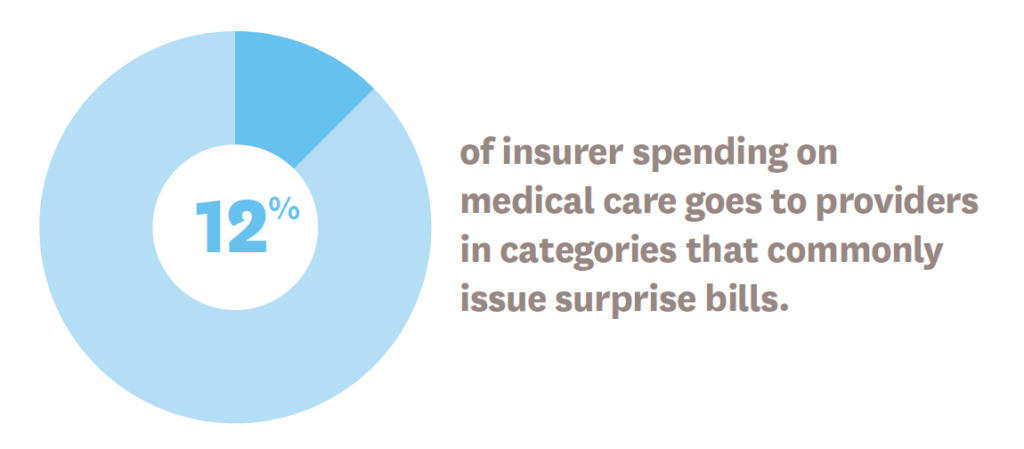
In one study, Erin L. Duffy, a Schaeffer Center postdoctoral research fellow, and her co-authors found that 12% of insurer spending on medical care goes to providers who commonly issue surprise bills.
Loren Adler, associate director of the Schaeffer Initiative, provided technical assistance to state leaders in Indiana, Maine and Virginia in crafting surprise billing legislation in 2020—with Indiana passing the first state law to protect patients enrolled in self-insured employer health plans.
Ginsburg, Adler and other initiative leaders have also provided guidance to the U.S. Congress on this issue. As a result, in December 2020, Congress passed legislation that eliminates surprise bills for patients who receive emergency care, are transported by air ambulance or receive nonemergency care at an in-network hospital. Adler was subsequently quoted in numerous media outlets.
“The law really captures every single form of surprise billing that we think of in this context, except ground ambulances,” Adler told The New York Times.
With renewed support from Arnold Ventures through 2023, USC-Brookings Schaeffer experts will continue the team’s solution-focused work on surprise billing.
Regulatory gaps lead some Americans to choose health insurance that falls below the standards set by the ACA.
Building on decades of prior law, the Affordable Care Act (ACA) took important steps toward a comprehensive regulatory structure that sets minimum standards for healthcare coverage. Yet some plans—referred to as “junk insurance”—still fail to meet those standards, leaving consumers burdened by high costs.
In addition to conducting an expansive analysis of junk insurance, Schaeffer Initiative Fellow Christen Linke Young has met with staff from numerous congressional committees and state insurance departments to offer pathways to improved regulation and oversight. After a yearlong investigation into the issue, the House Committee on Energy and Commerce released a report on short-term plans to curb junk insurance, citing work by Linke Young and Kathleen Hannick, a Schaeffer Initiative senior research assistant.
Despite reports of cost reform by CMS, analysis reveals that savings were overstated.
The Centers for Medicare & Medicaid Services (CMS) estimated that the Medicare Shared Savings Program led to $2.6 billion in gross savings in 2019 and $1.2 billion in net savings when accounting for shared-savings payments to participating Accountable Care Organizations (ACOs). Alice Chen, a Schaeffer senior fellow, and J. Michael McWilliams, a Schaeffer Center visiting scholar, crafted a two–part response published in Health Affairs. They outlined the ways that the CMS assessment is misleading and recommended reforms to help ACOs achieve their potential and help CMS reach its efficiency goals.
“At this stage of Medicare payment reform, progress is not served by applauding illusory savings or overselling simple solutions such as downside risk,” they wrote. “Sound evidence and theory should inform vision and set a course. Resolve will be a must and patience a virtue. Guided by these principles, designing a payment system that improves the efficiency of care delivery, meets fiscal goals and makes patients better off should be doable.”
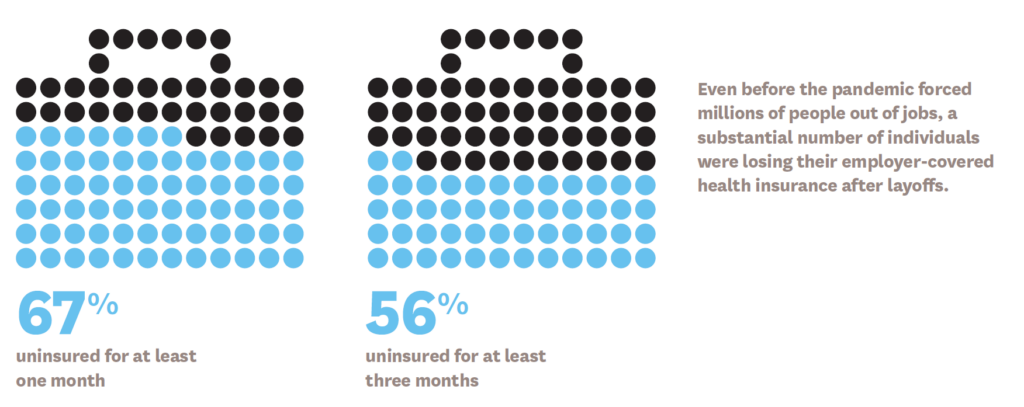
Employer-sponsored insurance is the primary source of coverage for U.S. workers and their dependents—so when unemployment rises so does the uninsured rate. Auto enrollment into subsidized coverage could be a solution.
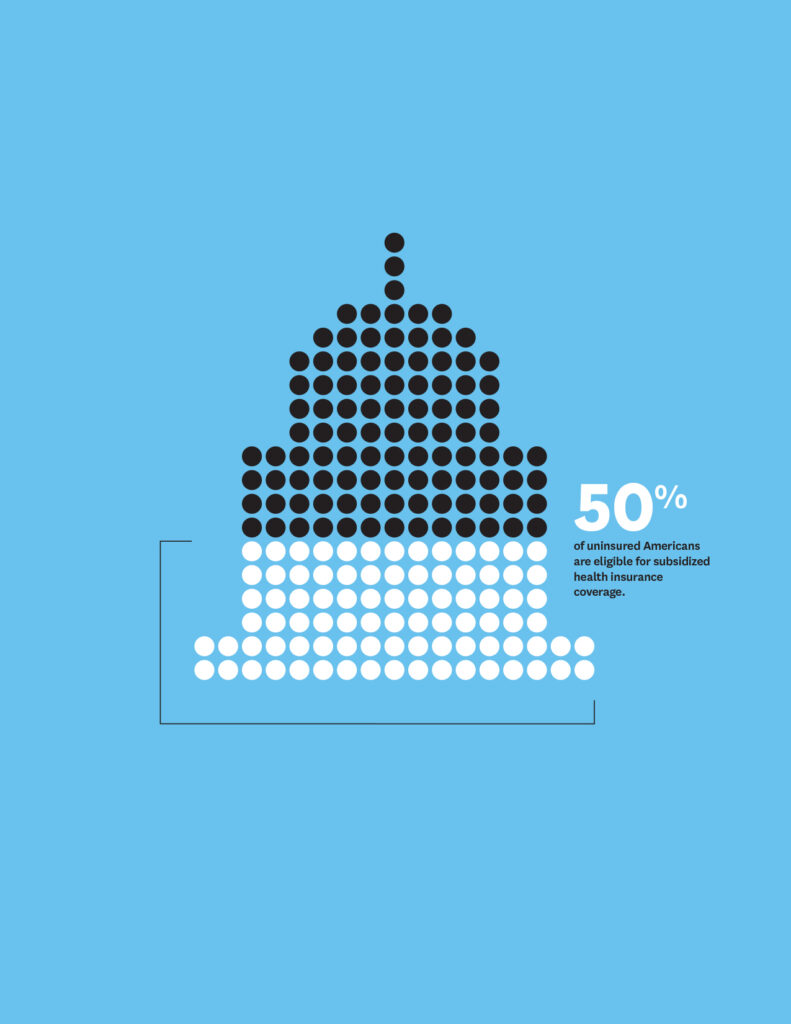
Millions of Americans who lose their employer-based insurance fall through the cracks. They might qualify for Medicaid or insurance through subsidized marketplaces created by the ACA but getting insurance through these sources requires information and action on the part of the individual. In an analysis published by Health Affairs, Linke Young and colleagues found two obstacles to enrollment that could be addressed through federal and state policies: perceived affordability of coverage and complexity of the enrollment landscape. They offered three ways to improve health insurance enrollment: simplified income rules, consumer assistance and automatic enrollment. Such approaches could increase health insurance coverage even during an economic downturn.
Linke Young continued her work on auto enrollment through additional publications, a webinar co-hosted by the Schaeffer Initiative and the American Enterprise Institute, conversations with members of Congress and a state auto-enrollment proposal with Covered California.
Schaeffer Initiative researchers launch a new portfolio of projects to improve understanding of rising healthcare spending.
With $3.6 million in support from Arnold Ventures, the team will take a data-driven look at provider prices, market consolidation, private equity, consumer costs, and a patchwork of related state and federal laws to produce evidence-based insights for consumers, insurers and policymakers.
The researchers hope to fill knowledge gaps that have prevented action or led state and federal policymakers to pursue ineffective solutions.
You must be logged in to post a comment.