Medicare and Medicaid
Our work in Medicare and Medicaid
-
Medicare Advanced Imaging Payment: Dysfunctional Policy Making
Medicare’s experience of paying for outpatient imaging services, particularly expensive advanced imaging such as MRIs, CAT scans, and nuclear scans, has been tumultuous over the last 20 years.
Categorized in -
Will Medicare Run Out of Money?
Join the Bipartisan Policy Center, the American Enterprise Institute, and the USC-Brookings Schaeffer Initiative for Health Policy for a panel discussion with congressional staff and experts to examine policy options that can avert the worst outcomes and place the Medicare program on a better track.
Categorized in -
Schaeffer Solutions: Health Policy Recommendations for the Biden Administration and 117th U.S. Congress
The USC-Brookings Schaeffer Initiative for Health Policy has developed practical recommendations and analysis in a number of critical policy areas.
Categorized in -
Medicare Payment for Physician-Administered (Part B) Drugs: The Interim Final Rule and a Better Way Forward
A look at how policymakers can reform an interim-final rule to use Medicare’s demonstration authority under the Center for Medicare and Medicaid Innovation (CMMI) to make large reductions in the amounts it pays physicians for high-cost medicines they administer under Part B.
-
Monthly Cost Sharing Doubles Throughout the Year for Some Medicare Insulin Users
Schaeffer Center researchers examined how use of insulin changes as cost-sharing fluctuates over the course of the year for Medicare Part D beneficiaries.
-
Without Reform, Medicare Policies Will Hamstring New Gene Therapies
It took until the fall of 2020 – three years after FDA approval – for Medicare to consistently pay an adequate amount for CAR-T therapy.
Categorized in -
How Can the Biden Administration Improve the Medicaid Program?
The panel will examine options to improve Medicaid eligibility rules, enrollment processes, and benefit designs, as well as approaches that could improve the quality and efficiency of the care delivered to Medicaid beneficiaries.
Categorized in -
Association Between Race/Ethnicity and Disparities in Health Care Use Before First-Episode Psychosis Among Privately Insured Young Patients
Racial/ethnic disparities in health care use and clinical outcomes for behavioral health disorders, including psychosis, are well documented, but less is known about these disparities during the period leading up to first-episode psychosis (FEP).
Categorized in -
Associations of Intensive Lifestyle Intervention in Type 2 Diabetes With Health Care Use, Spending, and Disability
Is an intensive lifestyle intervention for type 2 diabetes associated with long-term health care use and Medicare spending?
Categorized in -
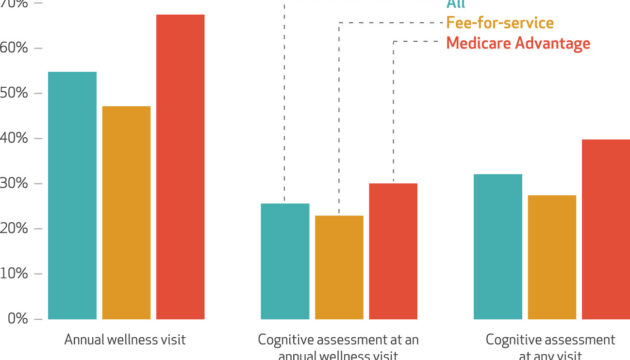
Cognitive Assessment At Medicare’s Annual Wellness Visit In Fee-For-Service And Medicare Advantage Plans
The study provides new insights – the self-reports of survey respondents – into cognitive assessments at annual wellness visits, an area that has been somewhat hidden from view.
Categorized in