
Explore our priority areas below ↓
The USC Schaeffer Center for Health Policy & Economics steadfastly pursues innovative solutions rooted in evidence-based research to measurably improve value in health. Our experts focus on work that informs lawmakers, media and private-sector leaders on pressing healthcare challenges and, most importantly, research that makes a vital impact on the lives of individuals everywhere.
With an extraordinary breadth and depth of expertise, our emphasis on four key areas helps ensure our efforts effectively improve health through better policy.
These are our priorities:
- Our experts lead the conversation on surprise medical billing.
-

Many patients who diligently seek providers from within their insurance networks still get stuck with massive medical bills in emergencies and other situations where choice is not possible. Such surprise medical billing can leave patients and families not only with the stress of recovery but also under financial strain.

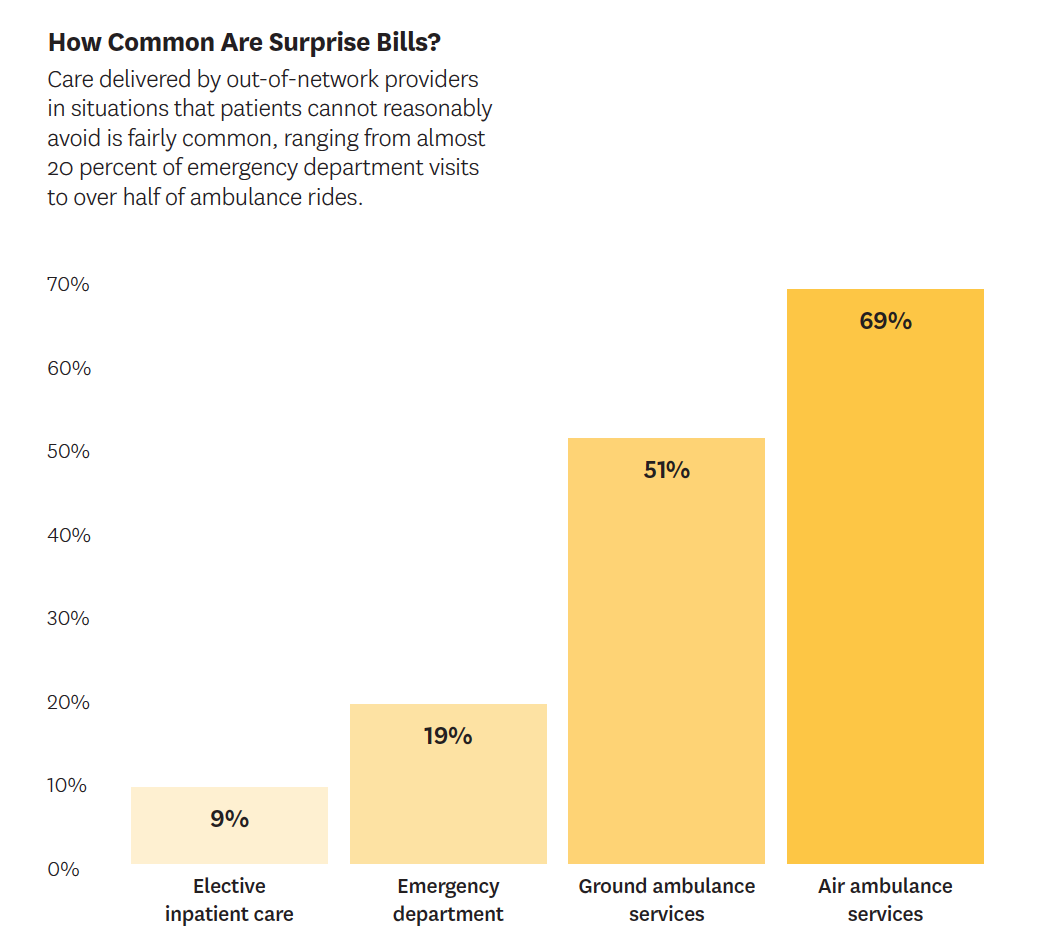
Emergency patients are usually taken to the nearest hospital, whether in-network or not. Across the country, approximately 1 in 5 ER visits involves care from an out-of-network provider and, in 15 percent of hospitals, patients are seen by at least one out-of-network provider in 80 percent of emergency cases.
Even for preapproved surgeries at in-network hospitals, patients do not choose every member of their care team. Hospitals select ancillary clinicians like anesthesiologists and radiologists, who may be out-of-network even though the hospital is in the patient’s insurance network.
While the insurer will typically pay a percentage of the charge for an out-of-network provider, it’s often far less than that provider’s list price. Patients get billed for the balance.
“As long as providers can charge whatever they please, the problem [of surprise medical billing] won’t go away.”
Loren Adler in
Kaiser Health NewsData show that specialties with the most opportunity to send surprise bills also have much higher list prices (as a percentage of what Medicare pays for those services) than other types of physicians. For instance, surprise medical bills from out-of-network anesthesiologists can be up to 344 percent of the Medicare reimbursement rate for that service.
Policymakers across the political spectrum agree on the problem’s urgency but disagree on its solution. To help build consensus grounded in evidence, experts with the USC-Brookings Schaeffer Initiative for Health Policy, a collaboration between the Schaeffer Center and the Brookings Institution, are at the forefront of analyzing this issue and the impact of proposed solutions. They have held one-on-one discussions with policymakers, given congressional testimony and authored numerous opinion pieces.
A pivotal February 2019 Schaeffer Initiative white paper clearly defined the market failures, backed by data and analysis. In addition, our experts — including Loren Adler, Erin Duffy, Paul Ginsburg, Christen Linke Young, Matthew Fiedler and Erin Trish — published 14 analyses on the topic and proposed numerous solutions in 2019. Combined, they garnered more than 500 media mentions, including in The New York Times and The Washington Post and on NPR. Seven federal agencies and committees requested their expertise as Congress weighed options.
The research revealed that surprise medical bills are most likely to come from emergency medicine physicians, anesthesiologists, radiologists and pathologists. Our experts also noted that ambulance services are often overlooked in legislation to address surprise billing but increasingly are cause for concern. More than half of ambulance rides are out-of-network, according to their findings. While such services once were provided either by local government or by hospitals for amounts close to the Medicare rate, new for-profit ambulance companies prefer to remain out-of-network so they can charge significantly higher rates.
Many of the federal proposals rely on solutions previously implemented at the state level, including in New York and California, which took drastically different approaches. New York set up an arbitration process based on billed charges to determine payment. In contrast, California used average contracted rates as a benchmark for payment negotiation.
Schaeffer Initiative experts were the first to provide analysis and insight on the effects of these different solutions. They noted that the law in New York actually increased overall healthcare spending.
As policymakers in both the House and Senate deliberate changes, they rely on Schaeffer analysis on the potential impacts for patient pocketbooks and society overall. Current policy proposals prohibit billing by out-of-network emergency and facility-based providers, but intense debate lingers in Congress about how to negotiate the final price paid. Our experts continue to respond to new legislation as it is proposed, highlighting potential unintended consequences of new changes to the bills.
- Delivery of high-value care varies significantly.
-
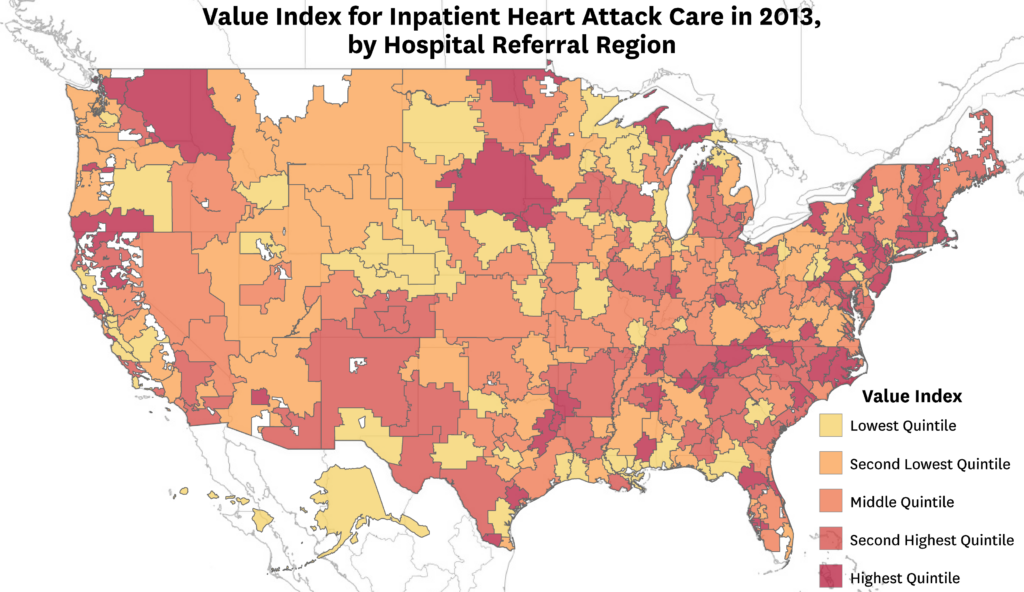
Improving value is central to reform, but measuring value is surprisingly complicated. John Romley and colleagues have formulated a novel framework for measuring variations in inpatient quality and cost of care, providing a blueprint to measure value in care delivery. They analyzed data on more than 33,000 fee-for-service Medicare beneficiaries admitted with heart attacks to 2,232 hospitals in 304 hospital referral regions in 2013. The team compared survival rates to total treatment costs, accounting for patient severity and socioeconomic factors, and found significant variation. Hospitals in the 90th percentile delivered 54 percent more high-quality stays compared to those in the 10th percentile. The findings may help achieve higher quality, lower costs — or both.
- We can better inform patients to improve private-sector care globally.
-
The private sector plays an important role in healthcare for low- and middle-income countries — but much of that care remains poor in quality. Neeraj Sood helped decode the causes of this marketplace failure, including why patients rely on less skillful providers and what impact cost has on decision-making. The study builds on Sood’s earlier work as an expert health economist for a report issued by the National Academies of Sciences, Engineering and Medicine spotlighting the poor quality of healthcare in developing nations.
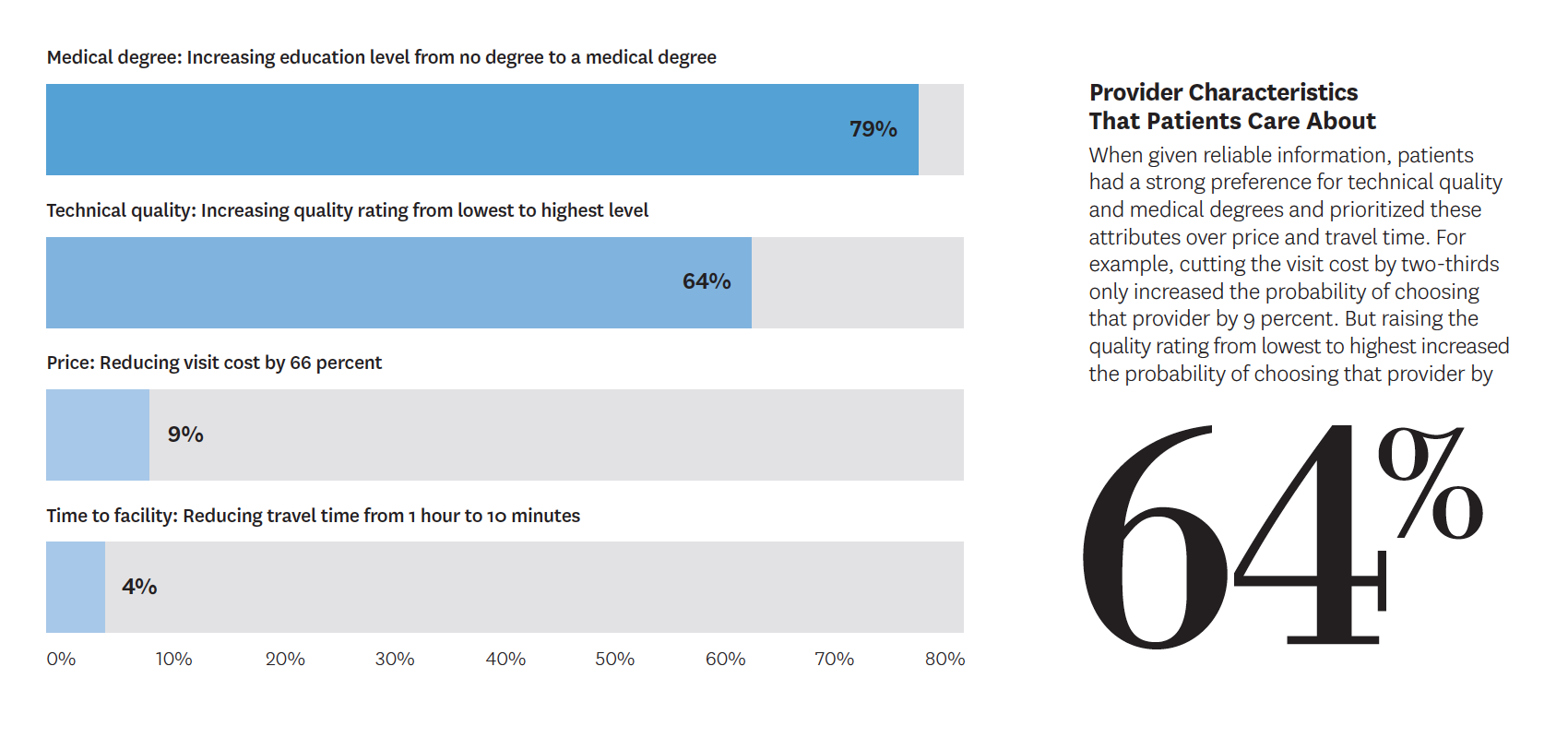
Conducted in India, the new project looked at the example of using failed treatments instead of the cheap yet effective technique of oral rehydration therapy for children with diarrhea-related dehydration. One hypothetical analysis asked parents to choose between two providers to discern the service characteristics they most value while another involved actors portraying parents of children with diarrhea or pneumonia to assess associations between levels of quality and provider fees.
Findings showed that, while people are indeed willing to pay more for good care, they often have difficulty distinguishing what constitutes technical quality. Without reliable quality information, patients prized observable factors — like positive interactions and longer appointments — rather than attributes such as correct diagnoses and proper treatments, which actually improve outcomes but are less visible.
“Thousands of deaths could be prevented and spending on unnecessary treatment spared if we could improve quality of care in low- and middle-income countries.”
Neeraj Sood and colleagues, working paper in the National Bureau of Economic ResearchWhile the quality of care may be lacking overall in India’s private sector, many physicians are capable of providing service of a better technical quality. For example, more than 70 percent of providers surveyed indicated that they would provide oral rehydration therapy — although only 13 percent actually did so in practice. Better incentives for physicians may remedy this discrepancy. Providing more information to consumers may also incentivize improvement in quality of care.
Sood and his co-authors suggest that more must be done to educate consumers about quality healthcare. Options include posting letter grades as is done for restaurants or developing mobile apps. Whichever strategies are used, the public sector should do more to provide information on improving healthcare in the private market.
- Universal coverage can be a reality while reducing costs and improving quality.
-
At the request of the U.S. Senate Committee on Health, Education, Labor and Pensions, the Schaeffer Initiative and the American Enterprise Institute collaborated to propose joint recommendations to reduce healthcare costs and achieve universal coverage. Their suggestions centered on improving incentives in private insurance and Medicare, removing state regulatory barriers to provider market competition and promoting competition in the pharmaceutical market.
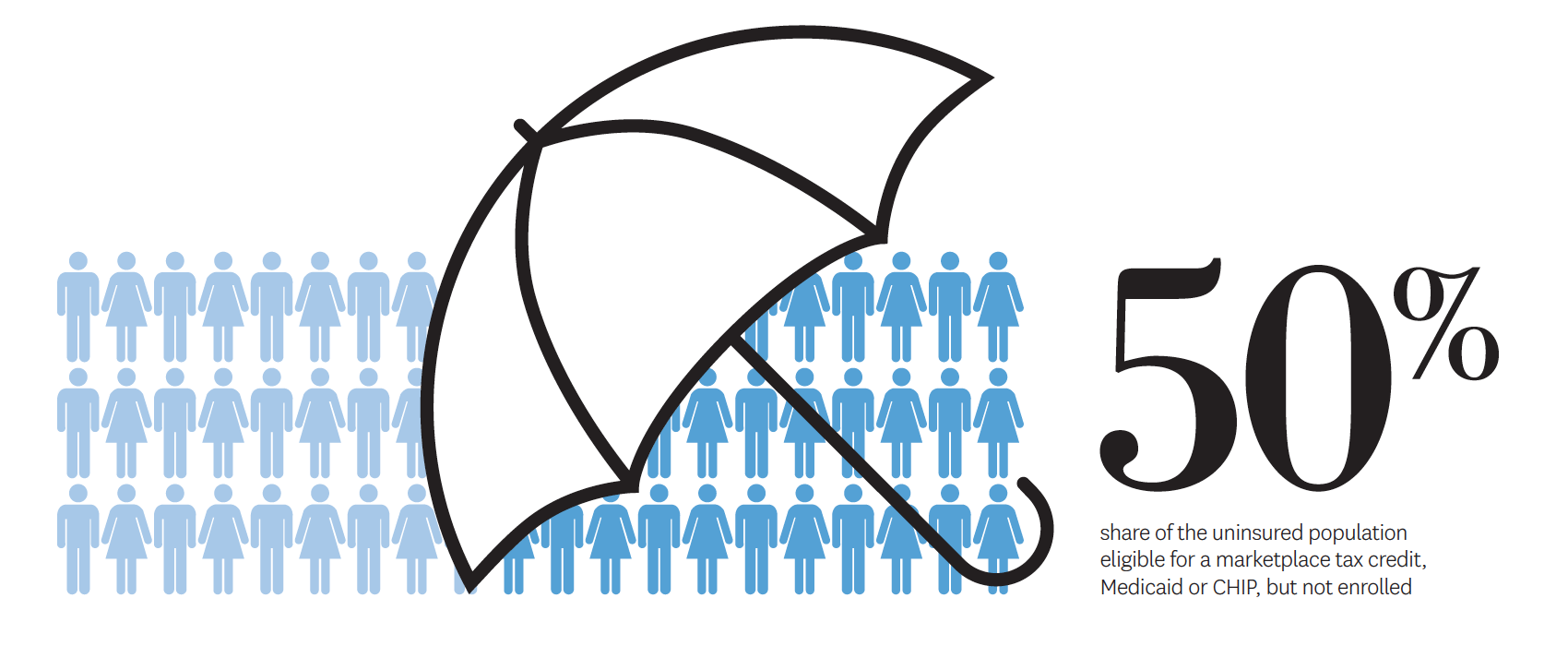
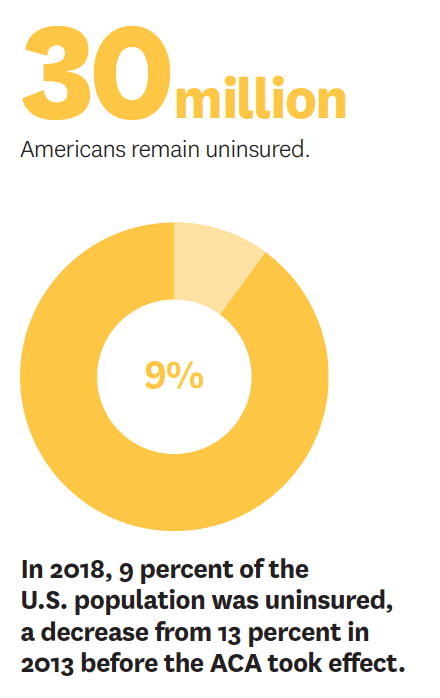
Schaeffer Initiative experts also authored a piece in the New England Journal of Medicine on how to build upon the Affordable Care Act (ACA). They discussed expanding Medicaid in all states, increasing assistance for buying private insurance, ensuring that people enroll in affordable programs for which they’re eligible and addressing coverage for undocumented immigrants.
An alternative recommendation is a plan costing the same as the ACA today — or less than a third to a quarter of the estimated annual price tags of Medicare for All proposals. The centerpiece would be universal catastrophic coverage for Americans not covered by Medicare, Medicaid or Veterans Affairs. These high-deductible policies would come from private insurers under federal contract.
Even though it vastly expands the number of people insured, the plan is cost-effective because it doesn’t cover all services all the time. However, high-value basic treatments such as preventive care, prenatal services and vaccines would be exempt from the deductible. The plan, developed by Dana Goldman and Kip Hagopian, varies the deductible based on family income — a feature not available in employer-sponsored plans.
Another alternative to Medicare for All, suggested by Geoffrey Joyce, is to harness the competitive forces inherent in Medicare Advantage while modernizing the bidding process and standardizing plans to improve efficiency. A limited set of Medicare Advantage plans would allow consumers to compare prices, facilitating competition on both price and quality. The approach is more politically feasible and more economically sustainable than expanding fee-for-service Medicare, Joyce concluded.
In other innovative research, Schaeffer investigators note the misalignment of incentives between insurers and patients with high-cost diseases like cancer — which leads many to distrust the private health insurance system. Goldman and Darius Lakdawalla suggest a way to rearrange priorities within the existing system by taking a cue from the life insurance industry.
“Consider an industry that excels in long-term planning and has a strong incentive to keep clients alive: life insurance.”
Dana Goldman and Darius Lakdwalla, op-ed in The Wall Street JournalAt the time of a cancer diagnosis, both the patient and her life insurer want her to live as long as possible because every month of added life postpones benefits and ensures additional premiums. In contrast, a health insurer wants to contain costs, which might mean limiting access to high-cost treatments. Partnerships between oncology care providers and life insurers may hold promise: Care providers could help patients identify and finance clinically appropriate therapies via their existing life insurance policies, creating a more effective and sustainable health insurance system, they write.
- Are generic drugs becoming too costly?
-
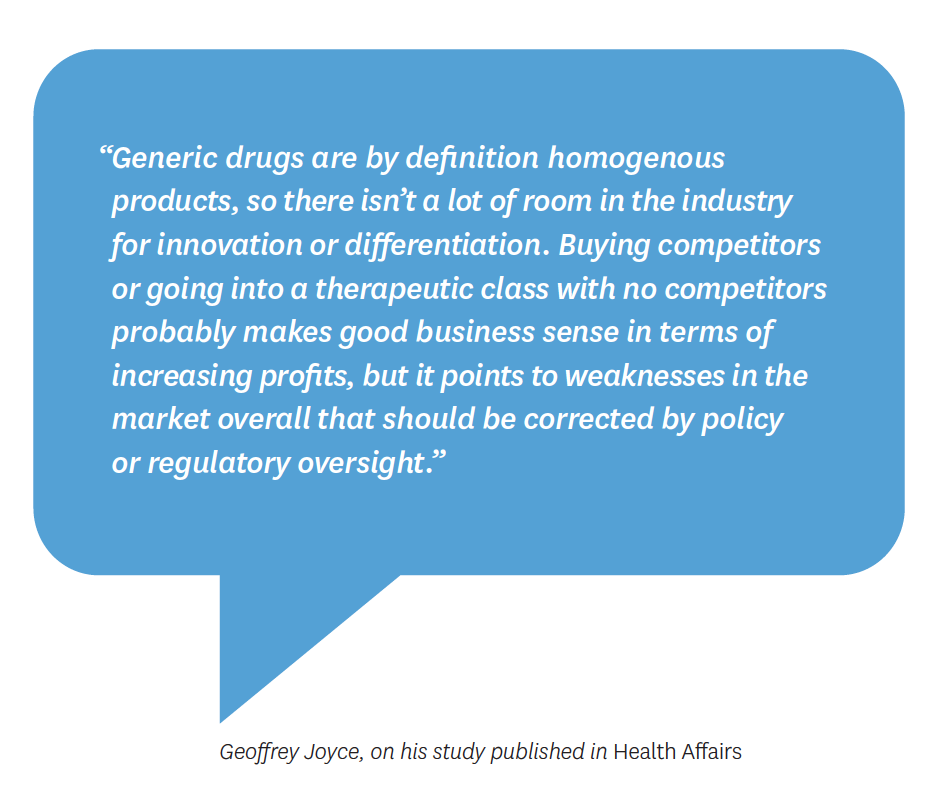
Generic drugs, which account for nearly 90 percent of prescriptions filled nationwide, have historically saved money for patients and the healthcare system — but Schaeffer Center research revealed that price spikes might indicate a market no longer functioning optimally. The study, led by Geoffrey Joyce, found that the portion of generic medications doubling or more in price annually represents a small but growing market share: from 1 percent of generic drugs in 2007 to 4.39 percent in 2013. For consumers, this can mean soaring costs for lifesaving drugs. Joyce suggests regulatory changes to spur competition and more rigorously analyze the impact of drug company mergers on generic pricing as corrective actions legislators might consider.
- Our researchers inform the federal and state drug pricing debate.
-

Voters across the political spectrum agree that reducing prescription drug prices should be a top congressional priority. Yet the challenge remains: how to control costs without removing the rewards that encourage medical innovation.
Medicare Part D, the federal program to help beneficiaries pay for outpatient prescription drugs, is at the heart of many recent federal proposals to address drug costs.
“The poor market dynamics of recent years and the perverse incentives in the supply chain must not stand in the way of a better drug policy for U.S. seniors.”
Erin Trish and Dana Goldman,
op-ed in STATDana Goldman wrote a piece for STAT evaluating one recent proposal that estimated $345 billion in Medicare savings over seven years, noting that, while it would reduce drug prices, it would also suppress innovation and could have long-term negative consequences on health.
From early debates about what a federal prescription drug benefit could entail to current discussions about high and rapidly rising prescription drug spending, Schaeffer experts have provided sound guidance, innovative research and evidence-based policy recommendations.

Recent work centers on how to restructure Part D’s benefit design to provide better financial protection for vulnerable consumers. Goldman, Paul Ginsburg, Geoffrey Joyce, Neeraj Sood and Erin Trish have shared research findings with the Centers for Medicare and Medicaid Services (CMS), the White House and committees in both houses of Congress to shed light on viable solutions.
They also have used the implementation of Part D to explore the effects of pharmaceutical marketing on prescribing patterns, the influence of the program’s growth on innovation trends, and the link between benefit design, formularies and medication adherence. To date, Schaeffer researchers have authored more than 25 studies that have been cited over 1,000 times, including in federal policy documents. In the last year, multiple legislative bodies reached out to Schaeffer experts to discuss proposed reforms to Part D.
Trish and Joyce wrote a body of work published in Health Affairs about how the increased use of expensive specialty drugs has ballooned spending related to catastrophic coverage, which kicks in after a beneficiary has spent a certain amount on prescriptions. Private insurance plans have little incentive to manage spending once the threshold is met because the government picks up 80 percent of the catastrophic tab. Therefore, more “skin in the game” is needed from these plans. Trish has met with congressional policymakers and CMS staff to propose solutions.
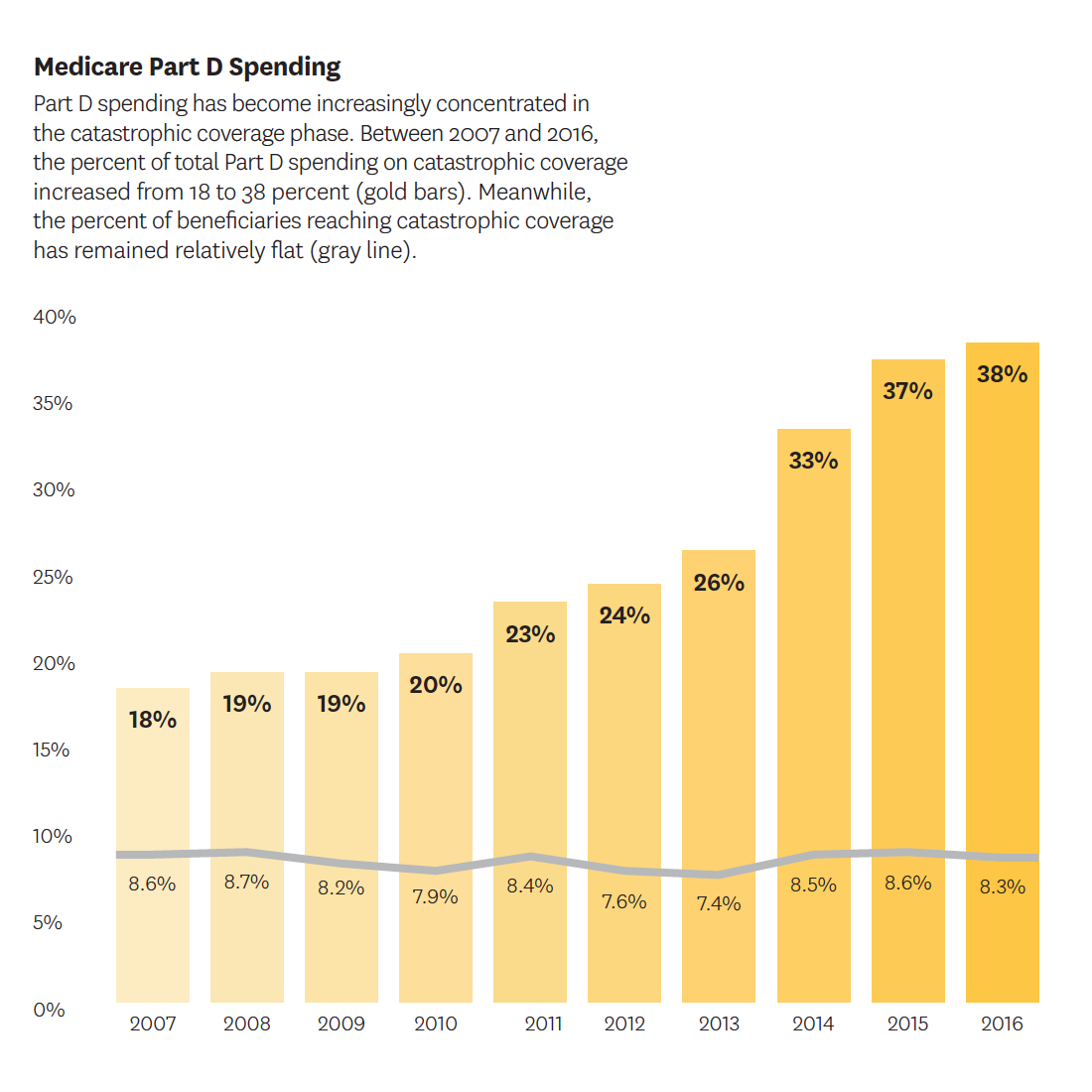
One potential answer — proposed by Trish in collaboration with Ginsburg, Joyce and Goldman in the New England Journal of Medicine — is to increase the financial stake of insurance plans, including liability in the reinsurance and coverage gap phases. These reforms could be coupled with changes granting plans greater flexibility in their use of formularies and transparency tools to speed progress toward more innovative contracting. Capping patients’ out-of-pocket costs is also important. Beneficiaries not receiving low-income subsidies are still expected to pay up to 5 percent of prescription drug costs during catastrophic coverage — which adds up rapidly.
Dissatisfied with the slow pace of policy reform federally, many states have moved ahead with drug pricing legislation, with 166 bills passed between 2015 and 2018. Sood co-authored a first-of-its-kind study of state drug pricing laws. He examined 35 state laws aimed at increasing drug price transparency. His finding: Only six states required more information than is already available, and no state has passed bills for tracking prices and profits at each link of the supply chain.
“The problem with all these bills is that they are shooting in the dark,” he wrote for The Hill. “A lot of information is available about drugs’ published list prices. But the drug distribution system is so complex — involving numerous middlemen and confidential negotiations for myriad rebates, fees and discounts — that manufacturers’ list prices are almost meaningless.” In response to this work, stakeholder and policymaker groups at the national and state levels have reached out to Sood to enhance the effectiveness of legislation related to drug prices.
- We are creating a new model for pricing drugs.
-
Drug manufacturers and health insurers rely on a price-per-dose model but this encourages high launch prices and access barriers that frustrate patients and providers. Alternative value-based reimbursement links pay to performance but it’s difficult to determine a drug’s long-term efficacy at its launch. Dana Goldman, Karen Van Nuys, Jakub Hlávka and coinvestigators proposed a different approach that ties prices to value but allows adjustments. Their three-part pricing would provide early access at a lower price while the drug undergoes further evaluation in a real-world setting. The result is increased access while still rewarding innovators. Other research by Jeff McCombs and Joel Hay explores value-based contracting and the dynamics of cost, value and innovation.
- What if prescription drug companies followed the Netflix model?
-

Across the country, states are grappling with growing populations with infectious disease, many of which disproportionately affect vulnerable populations who have the least access to care. An essential lesson from the early years of the HIV/AIDS epidemic is that early access to effective treatment not only improves health outcomes for patients affected but also avoids long-term costs. The bottom line is that widespread screening for infectious disease — and then treating those at highest risk — is cost-effective.
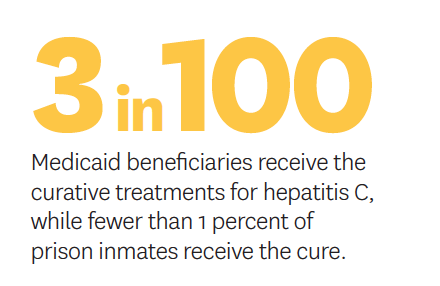
Today, approximately 20,000 Americans die from hepatitis C annually. That is more than the combined death toll from 60 other infectious diseases (including HIV). Unlike other public health challenges, a cure has been on the market for years, but the high cost puts it out of reach for many who have the condition. Fewer than 3 in 100 Medicaid beneficiaries and fewer than 1 in 100 prison inmates have received the treatment.
In his work on a National Academies of Sciences, Engineering and Medicine committee, Neeraj Sood and colleagues found that if 85 percent to 95 percent of people with hepatitis C were treated, the disease would be eliminated as a public health problem.
“It’s time to implement this pricing model in healthcare. It can lead us out of our prescription drug crisis by bringing universal access without breaking the bank.”
Neeraj Sood, op-ed in The ConversationAs states struggle to provide access to treatment to those in need without busting their budgets, Sood and his co-investigators have shown how engaging a subscription model, instead of a price-per-pill model, can meet this challenge. Colloquially called the “Netflix model,” Dana Goldman first coined the term to describe a novel licensing strategy whereby a state agency or payer pays a lump sum for unlimited access to treatment.
This sort of subscription model could reach more patients and improve outcomes while saving money.
Inspired by Sood’s research, Louisiana has already instituted a modified version of the plan. The state pays an annual fee of up to $58 million, partially covered by federal funds. In return, the contracted manufacturer provides unlimited access to an effective hepatitis C therapy. Compared to the status quo, the model provides greater incentive to treat as many people as possible.
Other states have also been in discussions with the Centers for Medicare and Medicaid Services about obtaining the necessary approvals to develop such a program.
- We are developing ways to assess technology’s true value in healthcare.
-
Technological breakthroughs are pivotal to medical progress but are also a major driver of increasing prices. While health technology assessment (HTA) is considered an essential technique for evaluating the value and appropriate price of new treatments in nations with single-payer systems, its advantages have yet to be felt in our country’s fragmented system.
Schaeffer Center and the Aspen Institute are collaborating to help foster the future of HTA in the U.S. Co-chaired by Darius Lakdawalla, Gail Wilensky of Project HOPE and Peter Neumann of Tufts Medical Center, the project will convene experts on value assessment to develop practical policy recommendations for easing expenses while promoting medical advances.
In the partnership’s first white paper, Lakdawalla, Karen Mulligan, Jakub Hlávka, Desi Peneva, Martha Ryan and colleagues give historic context and consider what a U.S. HTA body could look like today. Such a program would face unique challenges, given the complexity of the U.S. healthcare system and the exceptional role the U.S. plays in innovation globally.
Writing for The Hill, Dana Goldman suggested that a previous HTA model in the form of the federal Office of Technology Assessment (OTA) is ripe for restoration. Created in 1972, the OTA used systems and cost-benefit analyses — along with market research and consensus methods — to provide objective reports on science and technology-related issues. Congress dismantled the agency in 1995, but, according to Goldman, a new OTA could focus on medical innovation to help derive the appropriate value-based prices of new technologies.
In an article for STAT, William Padula addressed the importance of using HTAs to prioritize and protect patients when restraining prices. Nations use HTAs to not only set terms for negotiating with manufacturers but also in defining the limits on how much will be paid for care in certain circumstances. This is not always to the consumer’s advantage. The United Kingdom, for instance, limits dialysis coverage for diabetic patients over age 60, while all Americans on Medicare are eligible to receive it if needed.
Padula also posits that an OTA-style agency could provide the U.S. with a much-needed official voice in international pharmaceutical pricing. U.S. involvement might lead to our embracing the positive attributes of some aspects of pricing used by other countries. It may also result in other nations understanding the extent to which the U.S. shoulders the costs of medical discovery — and convincing them to share some of the weight.
Even if funded by the U.S. government, this new agency must operate independently to be truly effective. But just as the original OTA generated reports that saved enormous amounts of taxpayer money, a new agency devoted to HTAs could prove invaluable in controlling current costs while stimulating future innovation.
- Measuring the value of lifesaving cancer therapies.
-
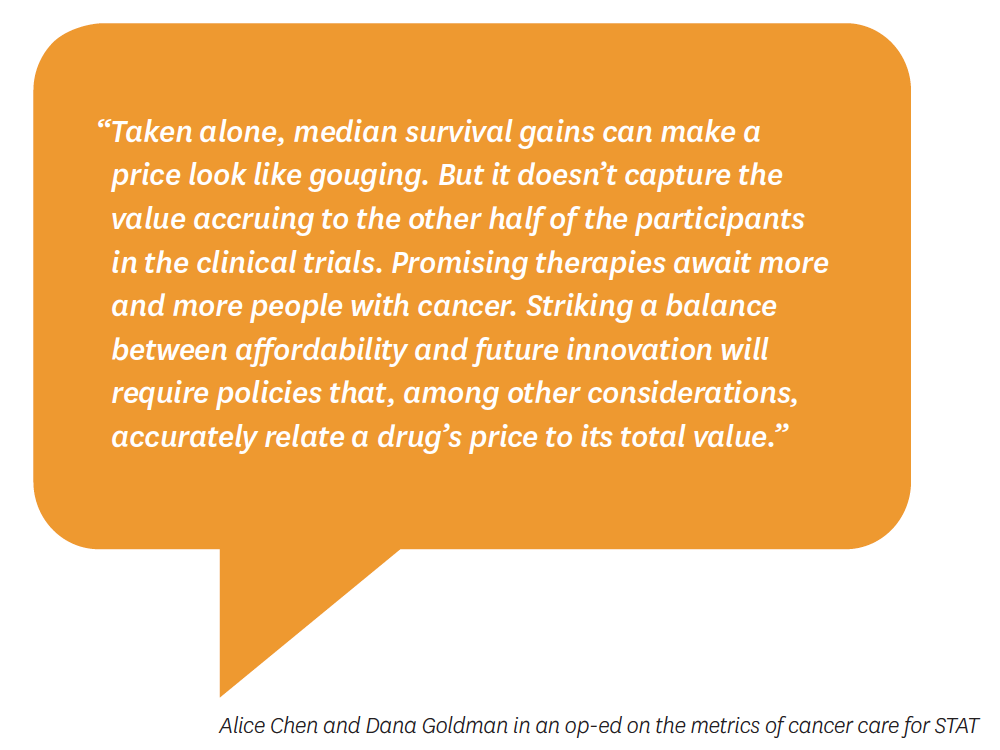
Cancer drugs with six-figure prices have sparked outrage, but are these new drugs measurably improving outcomes enough to justify the cost? A Schaeffer Center study cut through the controversy to gauge the true worth of these therapies. Conducted by a team including Alice Chen and Dana Goldman, the research found that these amounts are not as inflated as the accusations suggest.
The study assessed trends in price per health gains when measured by two widely used metrics, median survival and mean survival. While price per median survival gain showed large increases, price per mean survival gain increased much more slowly between 1995 and 2012. In recent years, price increases have reflected equally large growth in both metrics.
- Our investigators explore strategies for long-term well-being.
-

The U.S. has become a victim of its success in improving medical care. While Americans are living longer, those added years are not necessarily being spent in good health. Disability rates are rising, due largely to the high levels of disease among our elderly. In addition, mental illness is too often neglected — and, like other chronic conditions, can be expensive to treat when care becomes necessary.
Dana Goldman, Seth Seabury and Bryan Tysinger are examining the benefits — and costs — of chronic disease prevention to find the most viable strategies for long-term well-being. The challenges are enormous and urgent. Personal healthcare costs extract more than $2 trillion from our economy every year. Yet the U.S. ranks last among comparable nations on measures of healthcare system quality, efficiency, access to care, equity and lifespan.
Beyond the immense personal toll on individuals and families, more people are qualifying for senior entitlement programs and remaining in them longer, straining our national resources. Medicare spending alone is projected to almost double in the coming decades.
“Even without longer contracts, we could install a system that would reward plans for reimbursing care that was in the patient’s long-term interest, but not in the plan’s short-term interest.”
Dana Goldman, Seth Seabury and colleagues, chapter in the Aspen Institute Health Strategy Group’s report on chronic diseaseGoldman, Seabury and colleagues used the Schaeffer Center’s dynamic Future Elderly Model and Future Adult Model to discern the specific societal advantages of prevention. They examined the potential impact of such strategies on cardiovascular disease, serious mental illness and aging. In combating cardiovascular disease, the researchers estimated that following guidelines that include the simple, inexpensive intervention of taking low-dose aspirin would save almost 900,000 lives a year. Positive economic impact and increased life expectancy could also be achieved by early intervention in severe mental illness in young adults. Meanwhile, delaying the negative effects of aging could generate more than $7 trillion in health benefits if those senior years were productive.
Working with Tysinger, Goldman also used the Future Adult Model to gauge the fiscal impact of preventing cancer, diabetes, heart disease, hypertension, lung disease and stroke through 2050. Their analysis incorporated trends in demography, health behaviors and chronic disease to cast light on future disease burden, disparities, healthcare costs and the ramifications on federal programs. They compared a number of disease-reduction scenarios to estimate the effects of technological and lifestyle changes. They also factored educational attainment into their modeling to calculate how such changes might remedy socioeconomic disparities.
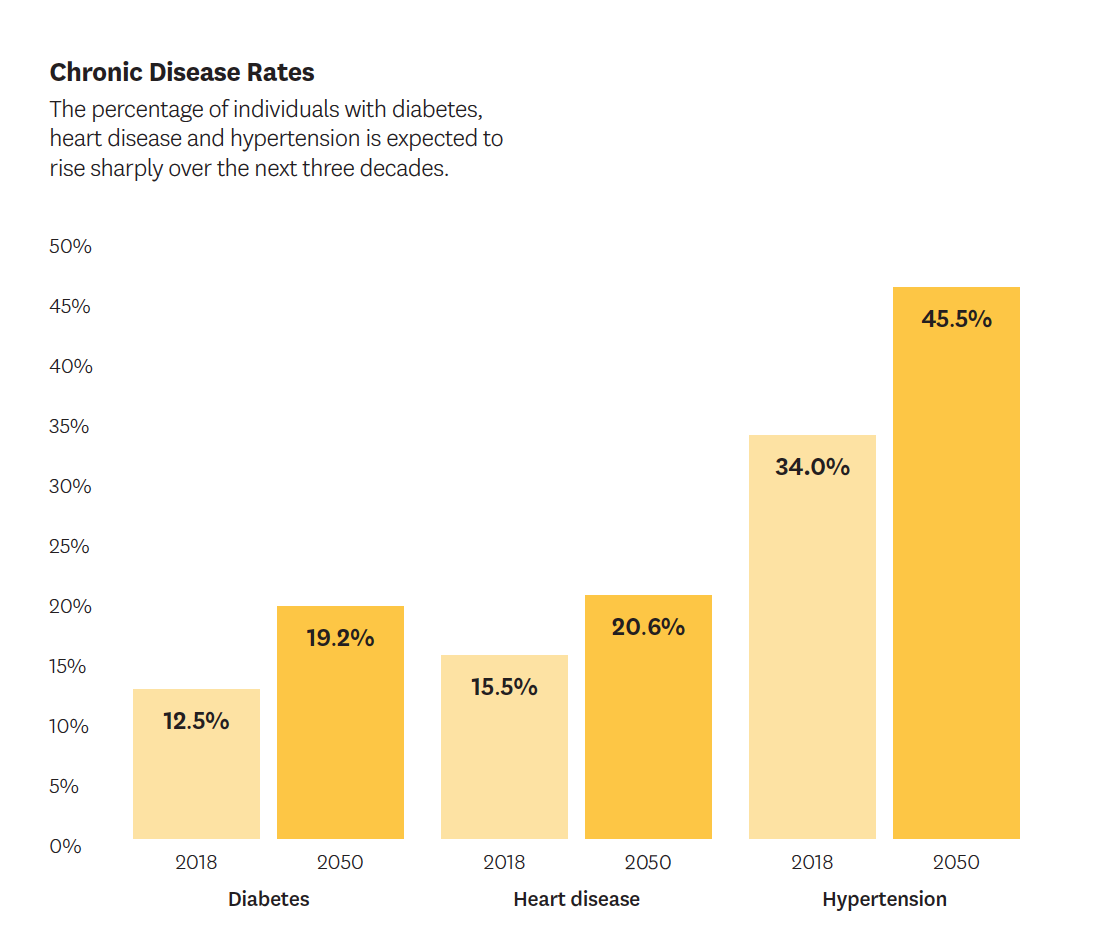
While the researchers acknowledge that eradicating chronic conditions is a lofty goal, they believe the explored scenarios are useful in demonstrating the financial benefits of disease prevention. In addition to reducing medical costs, successful interventions also would affect the labor supply, personal wealth, tax revenues and government spending.
Their research estimates that eradicating any one of the chronic conditions considered could result in savings of up to $3.5 trillion in current dollars when aggregated through 2050. This amount would offset federal subsidies for the Affordable Care Act. More important benefits would come in the form of longer, healthier and more productive lives.
The researchers note that, while progress in reducing the burden of chronic diseases depends on scientific innovation and lifestyle changes, the key to maximizing the impact of medical progress is moving to a model that rewards positive health outcomes rather than the use of healthcare resources.
They found “a disconnect between the ultimate payers (beneficiaries) and the intermediates who are doing our negotiating. At the end of the day, it is the employers and the government who decide what is going to be covered, not an insurer, and, as a society, we can decide that we want to start reimbursing for long-term health outcomes.”
As Goldman and Tysinger observe, this requires an increased focus on preventing disease rather than just treating it once it develops. To achieve this, patients and caregivers must change certain behaviors so that longer lives can be more independent, productive and enjoyed in better health.
- The benefits of extended-release formulations.
-
Even though correct doses are crucial to healthy outcomes, suboptimal medication adherence is all too common. In addition to undermining the effectiveness of chronic disease therapies, inadequate adherence costs the U.S. up to $289 billion annually. John Romley and colleagues examined the potential of extended-release formulations as a partial solution. Previous extended-release studies were limited to particular medications used for brief periods. Romley’s team investigated 15 extended-release treatments taken for more than a year. The findings showed better adherence — and improved health. For example, a 5.4 percent improvement in using preventive medications after myocardial infarction was associated with an 11 percent reduction in the rate of major vascular events.
- New evidence suggests policy changes that could improve kidney care.
-
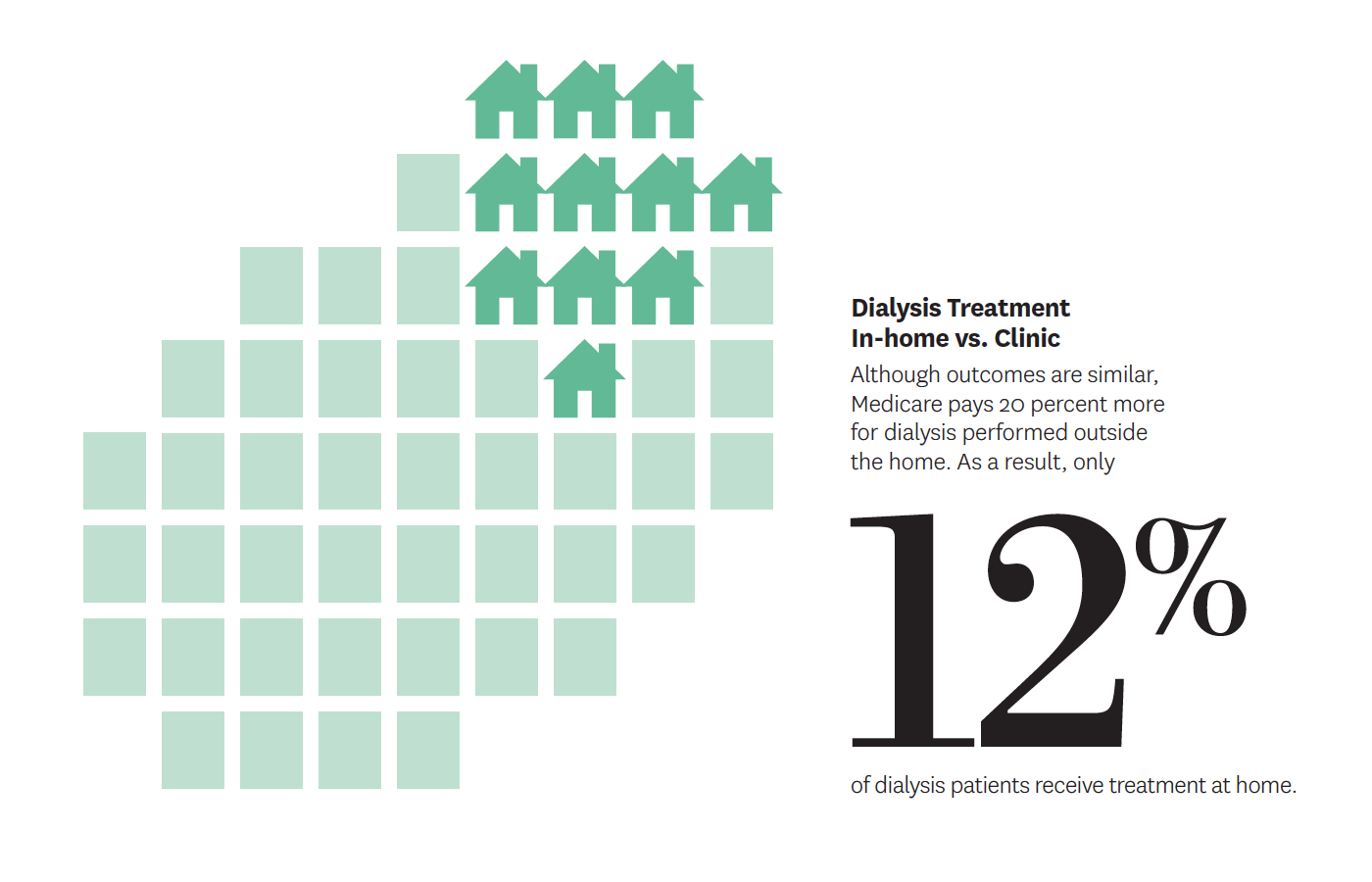
An estimated 15 percent of Americans will develop chronic kidney disease. Every year, more than 450,000 of these patients enter hospitals and clinics for dialysis to cleanse their blood. The high expense of this procedure and its disruptiveness to patients’ lives — especially when performed outside the home — garner considerable attention from regulators and doctors.
Medicare penalizes providers for 30-day readmission rates, assuming that providers can reasonably reduce rehospitalization by providing high-quality care. However, 30-day rehospitalizations are common in patients who receive dialysis and are more likely due to underlying disease burden than indicative of poor healthcare quality.
Although prior studies have identified major causes for 30-day readmissions in dialysis patients, few have assessed the clinical relatedness of hospitalization to kidney care. Nephrologist and policy researcher Eugene Lin and coinvestigators conducted a study that rectified this gap in knowledge. Their findings suggest that Medicare and other payers should refine readmission metrics to account for the actual relationship to dialysis as opposed to unrelated factors.
“Laudable goals could become dangerous mandates, and incentives that enhance care in one area could also reduce access to other essential services.”
Eugene Lin, op-ed in Morning ConsultWriting for Morning Consult, Lin also considered a recent federal initiative aimed at improving the lives of kidney patients while reducing costs. One much-needed aspect is increasing incentives for home dialysis. Currently, Medicare pays kidney specialists 20 percent more for dialysis performed outside a patient’s home than within it. As a result, only 12 percent of patients get home treatment, even though the outcomes are similar to in-clinic dialysis. Lin’s investigations demonstrate that even well-intentioned policies can be restructured to better help patients.
- We increase understanding and create solutions for the opioid crisis.
-
The opioid epidemic began with well-intended prescriptions for managing pain. As the crisis grew, many physicians remained unaware of its connections to their own procedures. Jason Doctor evaluated what happened when physicians found out about patients’ deaths from opioid abuse.
“One of the takeaways I’d like people to have is that doctors learn a lot of clinical facts but, when it comes to clinical judgment and decision-making, they fall prey to the same biases that we all do.”
Jason Doctor, in The Washington PostThe study, published in Science, involved 861 San Diego clinicians who prescribed opioids to patients who later overdosed fatally. Doctor’s team randomly selected half to receive a notification from the county medical examiner. The letter offered a supportive tone and information about safe prescribing guidelines.
Six state or city agencies have implemented the
nudge, notifying prescribers
of a patient’s fatal overdose.Within three months, opioid prescriptions from those receiving the letter decreased by nearly 10 percent compared to the group that did not receive the letter. They also were 7 percent less likely to start a new patient on opioids. These results are particularly promising given that numerous state regulations aimed at limiting opioids have shown little impact. In addition, Doctor’s interventions are easily scalable as existing state and federal resources already track drug overdose deaths. As a result, numerous states and city health departments are adopting his tactics.
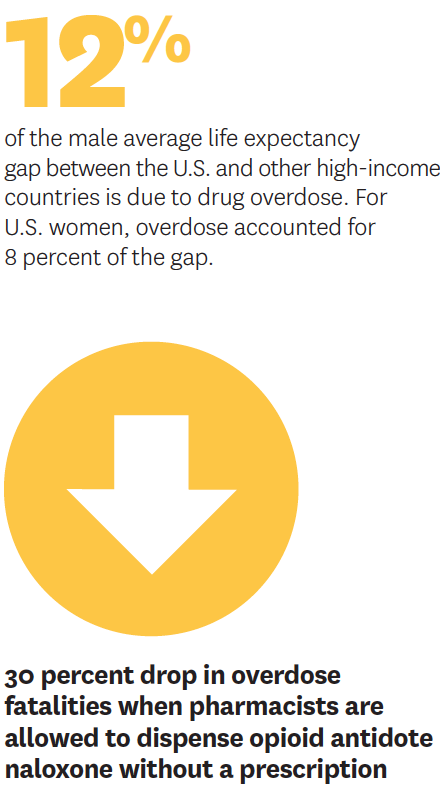
Rosalie Liccardo Pacula also evaluates the mechanics of the opioid crisis and how they influence the abuse of heroin, cannabis, and other illicit or addictive substances. She joined the Schaeffer Center in 2019, bringing with her the Opioid Policy Tools and Information Center (OPTIC). OPTIC is supported by the National Institute on Drug Abuse as a research center of excellence. Among other investigations, Pacula recently revealed that allowing pharmacists to sell the opioid antidote naloxone without a prescription was associated with a nearly 30 percent drop in overdose fatalities. Pharmacists have a key advantage in helping curb opioid abuse, she notes, because of their direct interactions with patients when filling prescriptions.
Pacula has presented her findings at the Centers for Disease Control and Prevention, National Institutes of Health, and in front of state and federal policymakers. She joins other Schaeffer Center researchers who are developing and evaluating strategies to combat substance abuse.
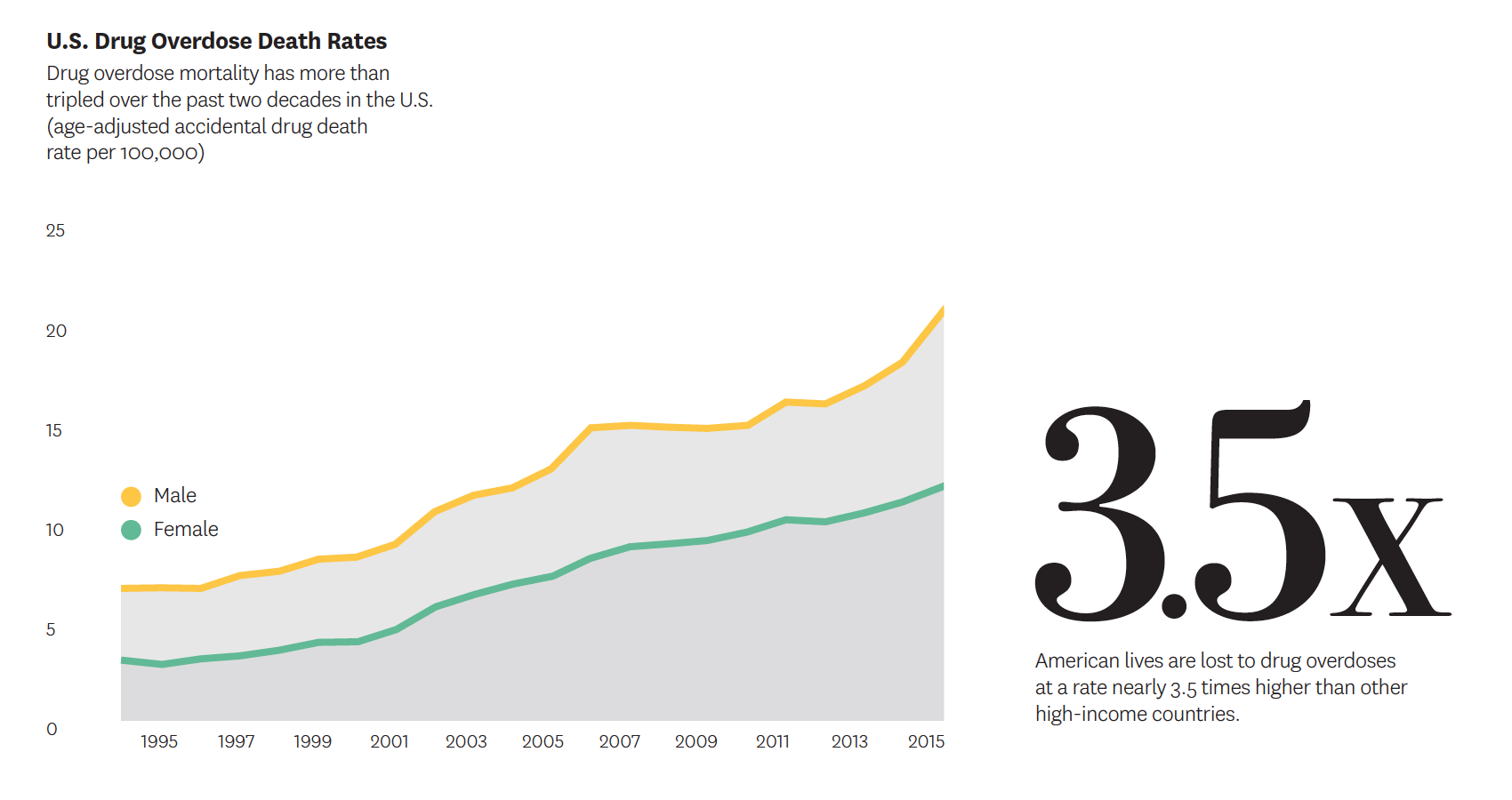
The need to find more solutions to this epidemic of addiction is urgent. American lives are lost to drug overdoses at a rate nearly 3.5 times higher than other high-income countries, according to research led by Jessica Ho. With data from 17 high-income nations, Ho’s study is the first to demonstrate the drug epidemic’s impact on widening gaps in life expectancy between the U.S. and the rest of the developed world. Especially alarming is her finding that U.S. death rates are 27 times higher than Italy and Japan, which have the lowest numbers of overdose fatalities.
In an influential book, Nobel Laureate Sir Angus Deaton calls these tragedies “deaths of despair.” His research suggests that they are accompanied by measurable deteriorations in economic and social well-being. Opioid and other substance addiction may therefore just be a symptom of larger issues that must be addressed to enhance community well-being.
- New quality protocols for pressure injury.
-
The national cost of hospital-acquired pressure injuries, also known as bedsores, could exceed $26.8 billion annually, not to mention leading to potentially fatal complications for patients, according to research by William Padula. His investigations center on quality-improvement protocols that can reduce both physical risks and financial costs. Padula’s findings suggest that hospitals should invest more in early detection and care — especially since Medicare penalizes providers for pressure injuries appearing after admission. The Department of Veterans Affairs has shown interest in implementing his recommendations. In addition, as treasurer of the National Pressure Ulcer Advisory Panel, Padula has provided testimony to the U.S. House of Representatives on his solutions for preventing such injuries.
- Keeping youth with mental illness in school accrues lifetime benefits.
-
Serious mental illness exacts devastating personal and financial tolls on those afflicted, their families and society. The relatively early age of onset exacerbates these costs, and it has long been assumed that early interventions lead to lifetime benefits in reducing this burden. However, little evidence existed to support this until groundbreaking research led by Seth Seabury.
The team, which included Sarah Axeen, Dana Goldman and Bryan Tysinger, employed Schaeffer Center’s Future Adult Model — an economic-demographic microsimulation — to examine the lifelong consequences of serious mental illnesses for people diagnosed before age 25. Simulation results demonstrate that these illnesses — which include psychoses, major depressive disorder and bipolar disorder — significantly worsen lifetime health outcomes, raise medical costs and reduce economic outcomes. For example, people showing serious mental illness by age 25 lost an average of nearly 10 years in life expectancy and $537,000 in lifetime earnings.
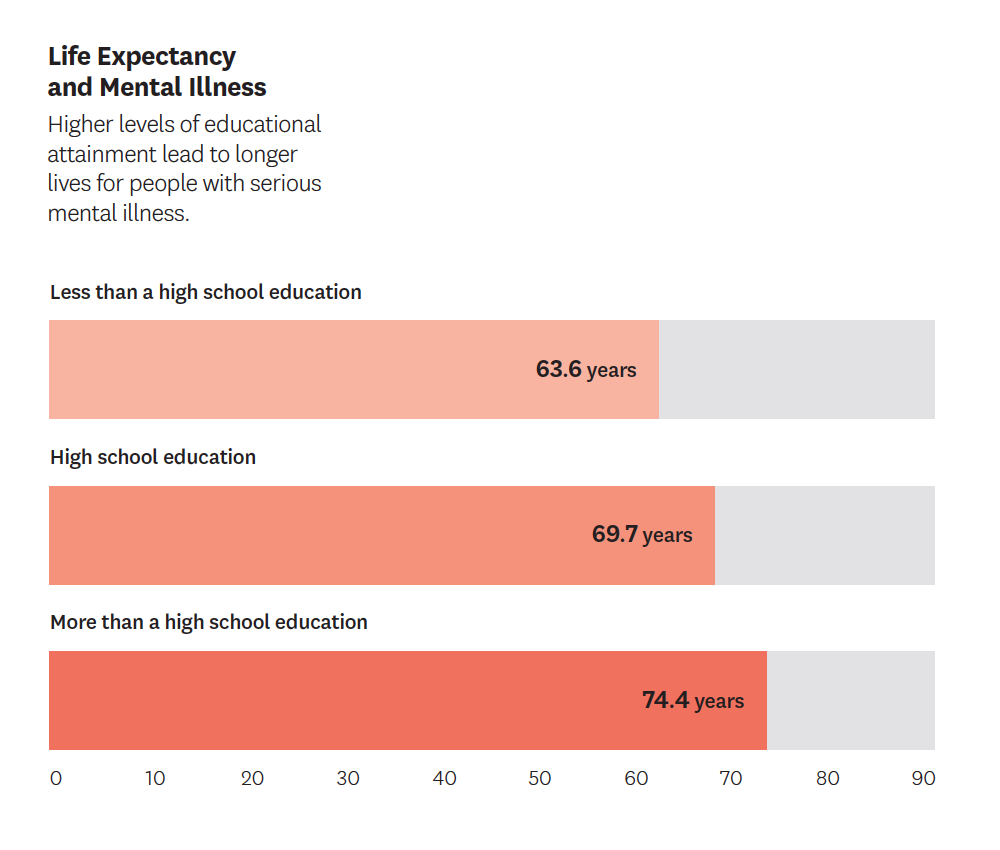
The study revealed that education has an outsized impact on the prospects of people with severe mental disorders.
Overall, the researchers conservatively estimated the lifetime burden to be $1.85 million for each patient — adding up to nearly a quarter of a trillion dollars nationwide for each new cohort. Significantly, this burden is unequally distributed, with the largest losses accruing to those with the worst educational outcomes.
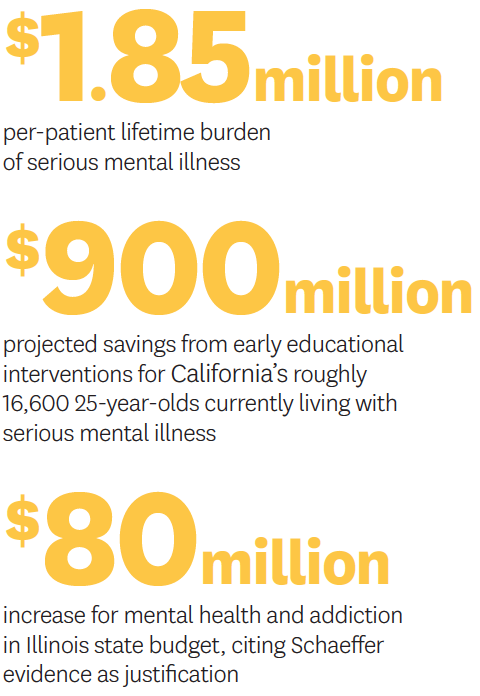
While interventions may seem costly, the study shows that a two-year educational intervention would produce an almost 2-to-1 return on investment. In California alone, early educational interventions would save more than $900 million over the lifetimes of the state’s roughly 16,600 25-year-olds currently living with serious mental illness. A 2019 poll by the California Health Care Foundation and Kaiser Family Foundation found that Californians’ top health priority was making sure people with mental illness can get treatment.
Although previous research showed the positive impacts of early identification, diagnosis and treatment on quality of life, the Schaeffer study is the first to assess the benefits of these interventions across individual lifespans.
“By spending more now to expand the behavioral health system’s capacity… we may be able to spot mental disorders early.”
Seth Seabury and Tom Insel,
op-ed in CalMattersSeabury presented the findings to policymakers and mental health advocates at a briefing at the Capitol in Sacramento. Schaeffer Center co-hosted the event with the Steinberg Institute, an organization founded by Sacramento Mayor and former State Senate President Pro Tem Darrell Steinberg to enhance policymaking related to mental health.
While reaching people with mental health issues — including those with behavioral disorders and substance addiction — remains a significant nationwide challenge, solutions must be found that address local and state concerns. To aid policymakers in assessing proposals to improve mental health treatment and access, Schaeffer Center — through the Keck-Schaeffer Initiative for Population Health Policy — is creating data chartbooks specific to individual states.
The data chartbooks provide key research and easy-to-understand statistics quantifying the magnitude of each state’s needs and challenges. The rigorously sourced findings describe the population with mental health disorders, the shortage of mental health providers, the impact on the healthcare system and the implications for the criminal justice system. This project is a collaboration with Behavioral Health + Economics Network (BHECON), which aims to unite diverse stakeholders to identify, examine and advance policy reforms to strengthen states’ mental health delivery systems.
State policymakers and stakeholders have found this data beneficial in improving policies related to psychological well-being. Illinois, for example, cited our research when instituting an $80 million increase in funding for mental health and addiction treatment. The state budget included $39 million for addiction treatment and prevention and $43 million for mental health services. This represented respective increases of 18 and 13 percent — as opposed to the previous year’s increase of just 3 percent. The chartbook produced for Illinois, which was presented at a stakeholder conference, found that nearly 25 percent of Illinois residents with serious psychological distress were not receiving needed help.
- Early childhood education breaks the cycle of poverty.
-
Nobel Laureate James Heckman used an extension of the Future Elderly Model to estimate the impact of early childhood education on lifetime health outcomes. Following data from low-income African-American children who participated in the noted Perry Preschool Project decades ago, his latest research looks at their outcomes at midlife — as well as their offsprings’ progress. Heckman, Duncan Ermini Leaf and colleagues found that those who participated in the program achieved significant gains that provided positive multigenerational effects on education, health, employment and civic life. Early childhood education resulted in stronger families and enhanced upward mobility for the next generation — an indication that early childhood education can be effective in breaking the cycle of poverty.
- We are revealing trends in access to dementia specialty care.
-
In the first large study to examine dementia diagnoses in older Americans over time, Julie Zissimopoulos and colleagues found that most patients never see a specialist. Using Medicare data to track diagnoses of nearly a quarter-million people over five years, the team found that 85 percent of individuals were first diagnosed by a non-specialist, usually a primary care doctor, and an “unspecified dementia” diagnosis was common. The researchers also found that the use of dementia specialty care was particularly low for Hispanic and Asian patients.
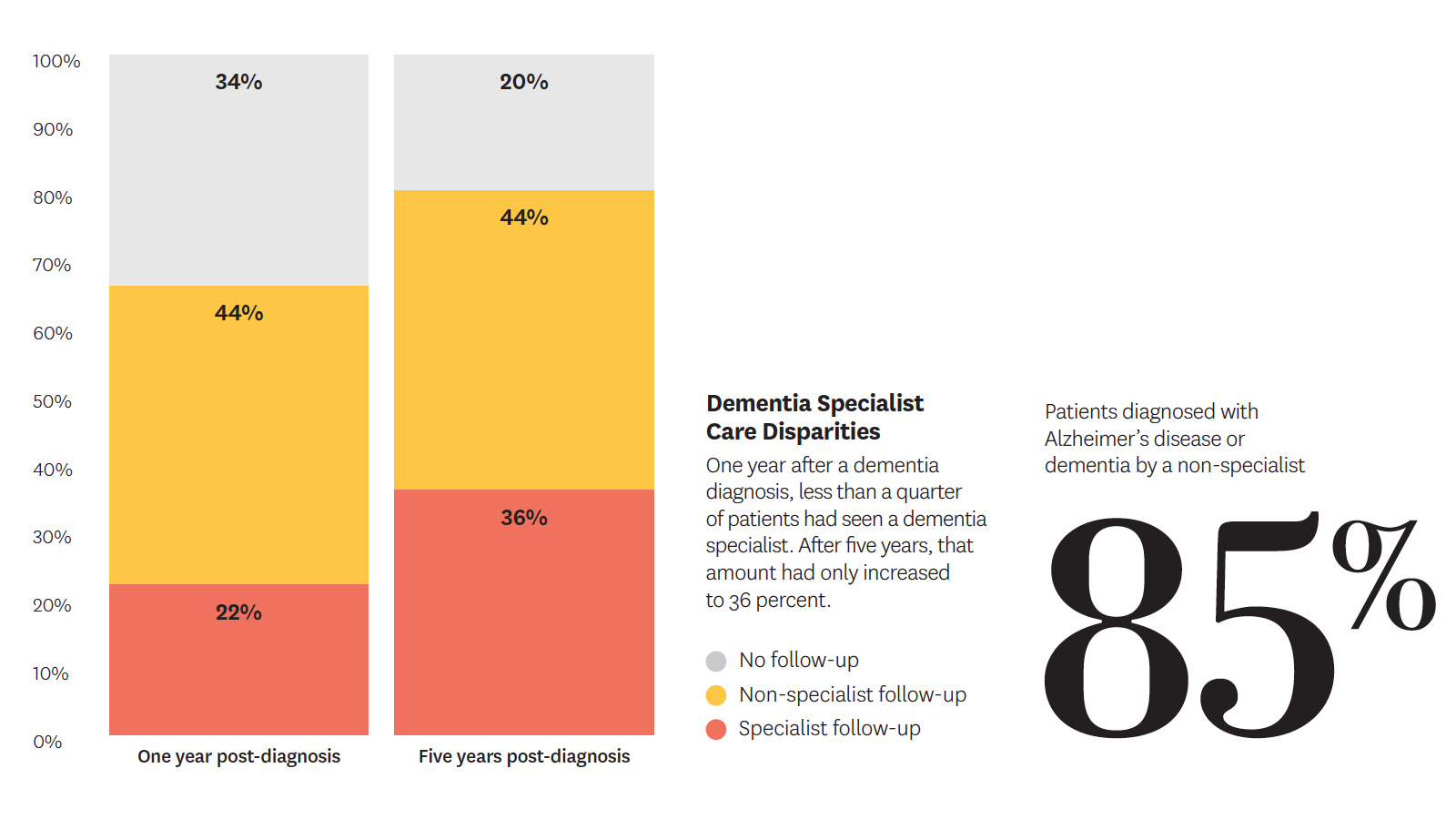
More accurate identification of dementia type may lead to better treatment, enhance knowledge of medications that may worsen symptoms, inform disease progression over time and encourage advance care planning.
“Dementia specialists are more familiar with subtypes of dementia and may be less likely to misdiagnose and wrongly prescribe medications to patients.”
Julie Zissimopoulos, study in Alzheimer’s & Dementia: The Journal of the Alzheimer’s AssociationIn other research, Zissimopoulos and collaborators have investigated possible new uses for old drugs as alternative approaches to Alzheimer’s specific pharmaceuticals that have failed to clear the beta-amyloid proteins linked to the condition. In two separate studies using large, national data sets, the researchers assessed antihypertensive medications and cholesterol lowering statins — used to fight heart disease — for potential impact on Alzheimer’s disease.
They found that certain types of both of these inexpensive medications hold the potential for preventing or delaying the onset of Alzheimer’s.
A nationally recognized thought leader in the field, Zissimopoulos was asked to join a National Academy of Sciences committee on Alzheimer’s and dementia. Together with Mireille Jacobson, she is also co-leading the Schaeffer Center’s new Aging and Cognition Project, which focuses on Alzheimer’s disease and related dementias, palliative and end-of-life care, and racial disparities.
- How does insurance coverage affect outcomes for vulnerable groups?
-
Cancer and diabetes are two of the nation’s leading causes of death, and low-income populations are especially vulnerable. Schaeffer Center researchers conduct vital studies on the impact of these diseases on both the insured and uninsured.
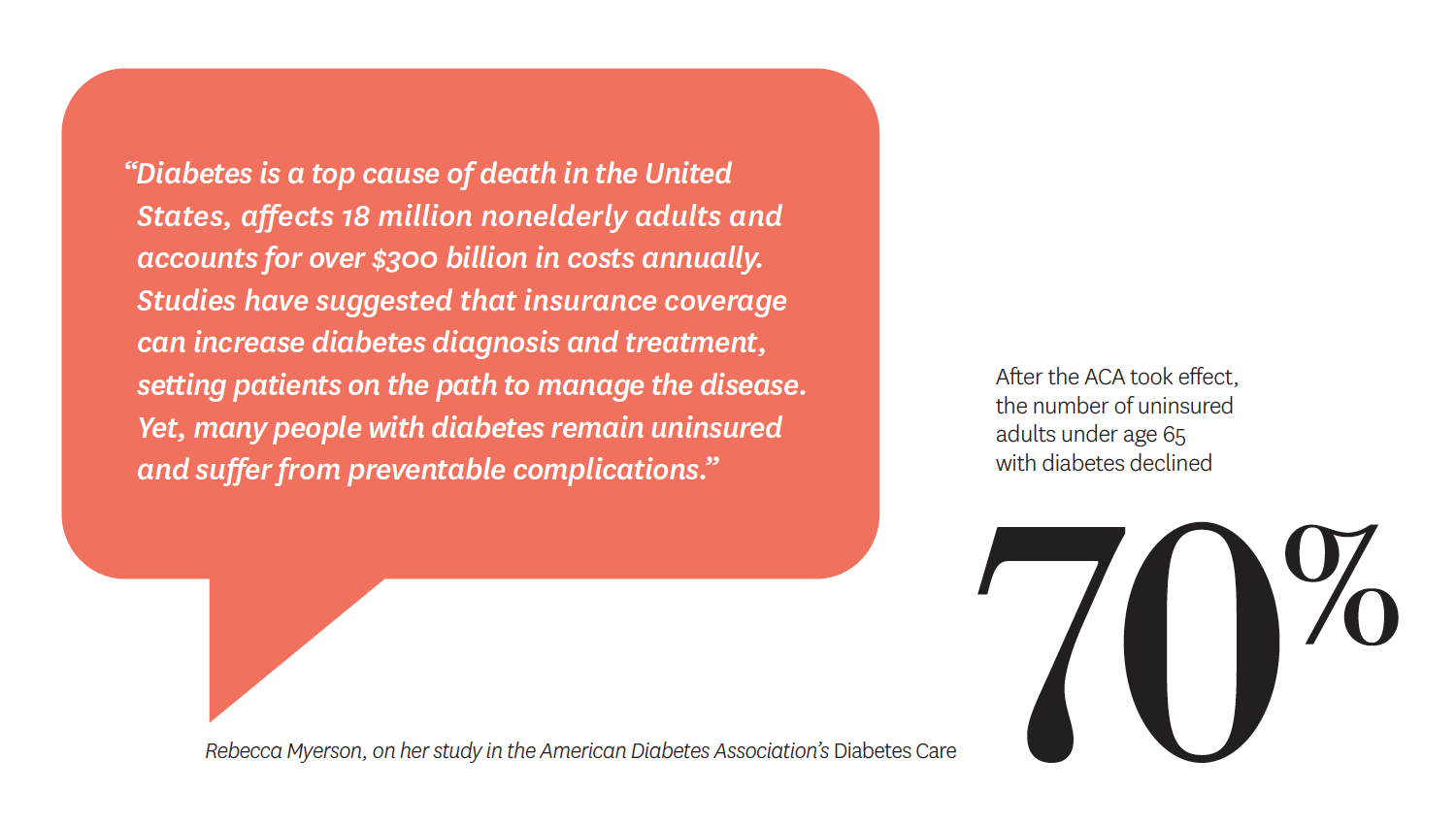
The Affordable Care Act (ACA), signed into law in 2010, significantly reduced the number of uninsured Americans. For diabetes patients alone, it expanded coverage for nearly 2 million people, more than half of them low-income. Research by Rebecca Myerson, John Romley and Dana Goldman analyzed the impact of the ACA
on diabetes patients.“Many people who have diabetes don’t know it. Access to insurance coverage through the ACA has helped this underserved population get diagnosed and access appropriate care.”
John Romley, on his study published in Diabetes CareThe team’s research found that, in 2009 and 2010, 17 percent of adults under age 65 who had diabetes were uninsured. After the ACA took effect, that number declined by 70.5 percent, from 17 to 5 percent. Among low-income adults with diabetes, the uninsured number declined by 27 percentage points. This study was the first to demonstrate gains in coverage under the ACA for patients with both diagnosed and undiagnosed diabetes.
Timely detection of certain cancers also significantly improves treatment options and health outcomes. However, access to screenings may be affected by lack of health insurance.
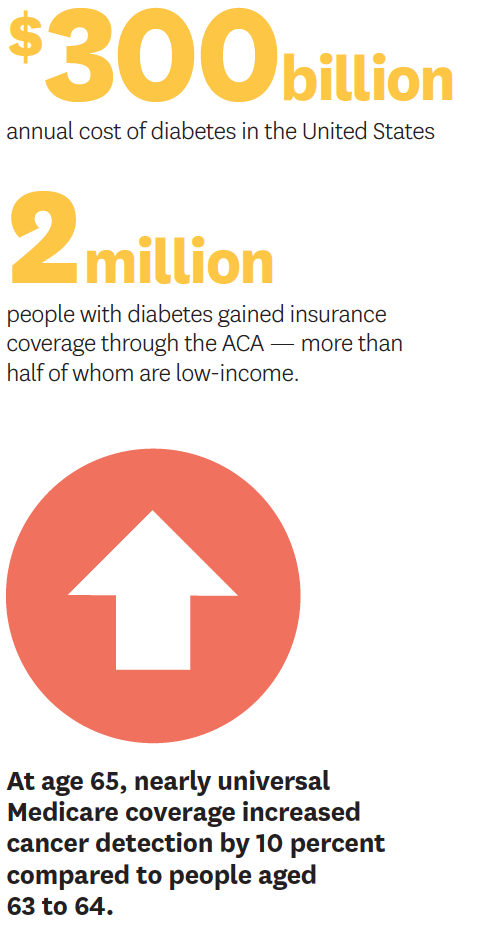
A study co-authored by Myerson, Goldman, Darius Lakdawalla and Reginald Tucker-Seeley examined whether Medicare — which provides nearly universal coverage for Americans beginning at age 65 — impacted cancer detection and mortality. They focused on breast, colorectal and lung cancer, for which screenings are recommended before and after age 65.
They noted that an initial year of treatment cost an average $73,000 for lung cancer and $28,000 for breast cancer in 2010 dollars. The elevated rates of bankruptcy among lung and breast cancer patients ages 50 to 64 suggest that out-of-pocket treatment expenditures may lead to substantial financial hardship for people lacking Medicare coverage.
Their report found a 10 percent increase in cancer detection among Medicare beneficiaries when compared to 63- and 64-year-olds not enrolled in the program. Detection increased more for women than for men, and the study also found differences by race. For example, black women experienced a particularly large jump in cancer detection — along with a decrease in mortality — at age 65. These estimates provide new evidence of Medicare’s impact on health outcomes for people in need of medical care.
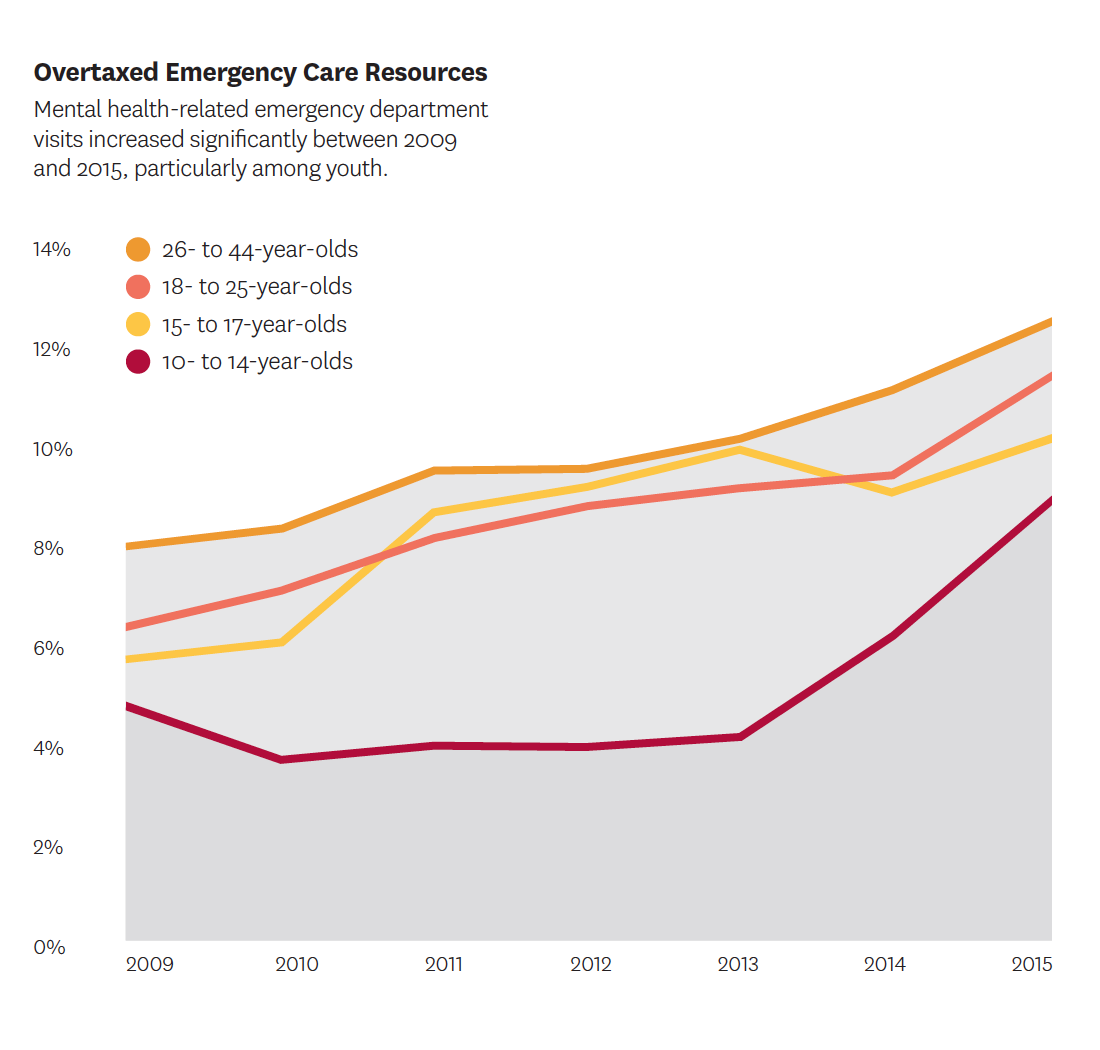
- Mental health needs and emergency care resources
-
Mental health-related visits account for a growing share of emergency department (ED) visits and resources. Research by Sarah Axeen and Michael Menchine shows the trend is driven largely by adolescent and young adult visits. For patients between 10 and 25 years old, annual growth rates for behavioral health-related visits were double those of older groups. Their findings also show that, because of longer patient stays, mental health-related visits use an increasingly disproportionate amount of ED time. The researchers urge more focus on acute mental healthcare and better understanding of needs by patient age group, with potential solutions including specialized psychiatric observation units, increased use of tele-psychiatry for emergency consultations and dedicated psychiatric emergency units.



You must be logged in to post a comment.