The COVID-19 pandemic resulted in many policy responses by public health officials in attempts to mitigate community spread. These responses generally fell into pharmaceutical and non-pharmaceutical interventions (NPIs). One such NPI that was used frequently was the shelter-in-place (SIP) policy, which was designed to reduce mobility and, therefore, the ability for the virus to transmit.
In this NBER working paper, Agrawal, Cantor, Sood and Whaley examine the impacts of SIP policies, both internationally at the country-level and in the U.S. at the state-level, on excess mortality.
The researchers focus on excess deaths– a measure that compares deaths from all causes in a given geography at a given point in time to expected deaths from all causes based on historical data. Through looking at excess deaths the authors capture both potential reductions in COVID-19 deaths and potential increases in non-COVID-19 deaths.
While emerging evidence has documented increases in excess deaths during the pandemic, the existing literature has not systematically examined the role of SIP policies in averting or contributing to excess deaths. Further, no studies have compared the impact of SIP policies between countries and compared these impacts within U.S. states.
Sood and his colleagues analyze data from 43 countries that implemented SIP policies along with all 50 states in the U.S.
They find that prior to the implementation of SIP policies, excess deaths were decreasing in most countries and states. However, following the implementation of SIP policies, excess mortality increases—a trend that continues for the length of the SIP policies. Across all countries, a one-week increase in the duration of SIP policies is associated with a 2.7 increase in excess deaths per 100,000.
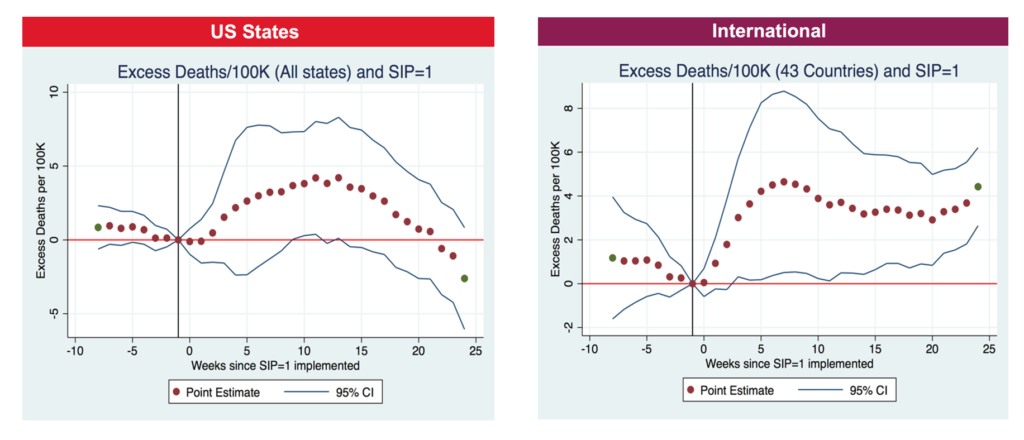
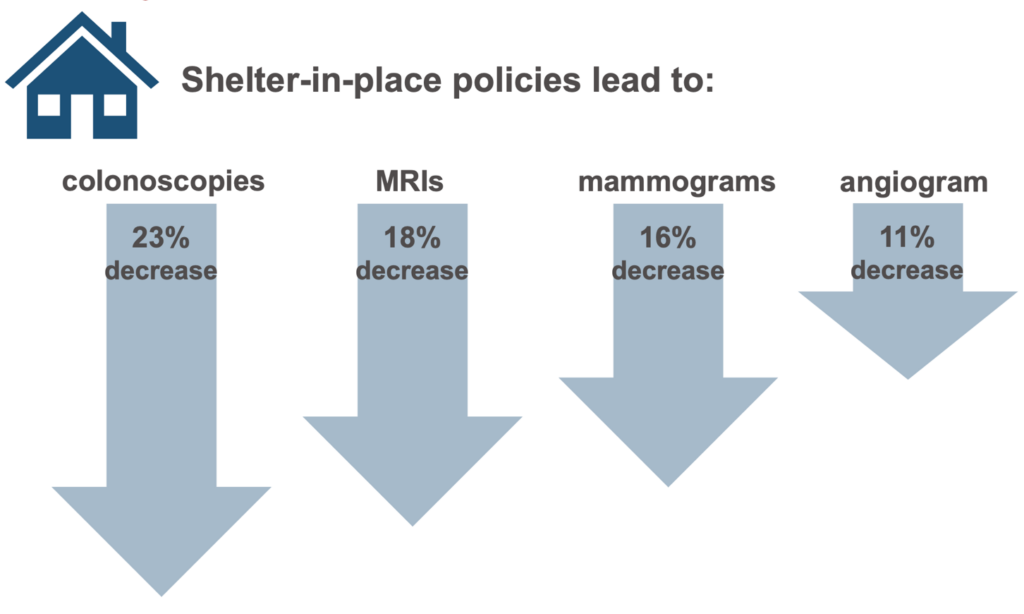
Over multiple analyses conducted, the researchers find similar trends. Taken together, their findings indicate that implementation of SIP policies does not seem to have met the aim of reducing excess morality. It is possible that people were already staying in place to avoid getting infected by the time SIP policies were implemented. It could also be possible that the potential increase in deaths is due to severe economic and social stress resulting from the pandemic. Finally, the researchers note that other studies have found SIP policies might have led to a reduction in non-COVID-19 care, which might contribute to an increase in non-COVID-19 deaths.
 Source: Cantor, J. H., Sood, N., Bravata, D., Pera, M., & Whaley, C. M. (2020). The Impact of the COVID-19 Pandemic and Policy Response on Health Care Utilization: Evidence from County-level Medical Claims and Cellphone data (No. w28131). National Bureau of Economic Research.
Source: Cantor, J. H., Sood, N., Bravata, D., Pera, M., & Whaley, C. M. (2020). The Impact of the COVID-19 Pandemic and Policy Response on Health Care Utilization: Evidence from County-level Medical Claims and Cellphone data (No. w28131). National Bureau of Economic Research.
Using these findings and potential explanations the authors conclude that continued reliance on SIP policies in this pandemic might not optimal. The authors discuss the importance of pharmaceutical interventions such as vaccinations and therapeutics as interventions that are likely to have large positive impacts. With this study, the authors contribute to the growing literature of the complex effects of SIP policies that can be used to guide future responses to a pandemic.
This study was published at NBER.

You must be logged in to post a comment.