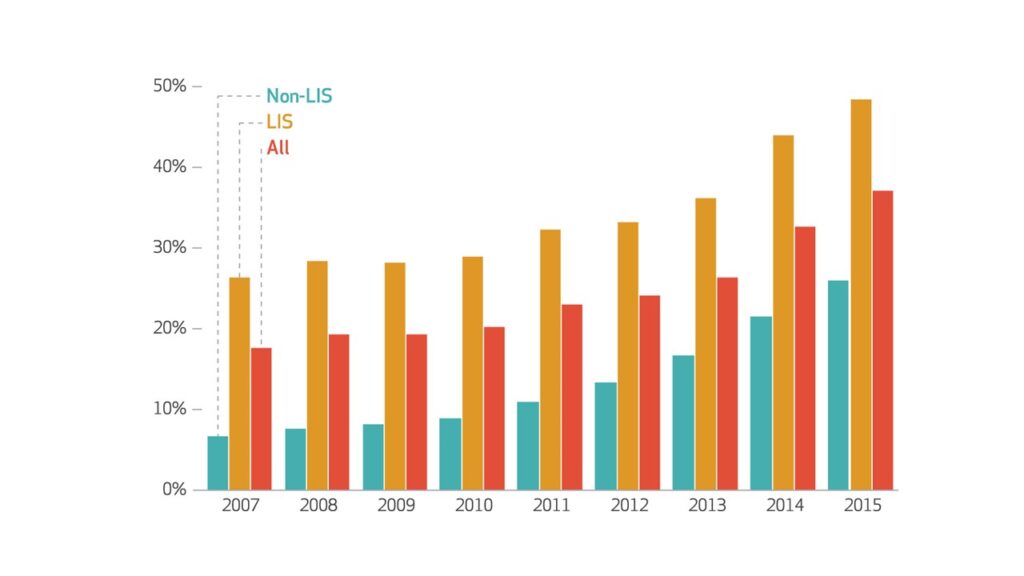
Medicare Part D currently lacks an out-of-pocket cap; instead beneficiaries with high prescription drug spending pay five percent on all prescription drugs once they reach catastrophic coverage. A recent study found that more than one million Part D enrollees who were not eligible for assistance with their out-of-pocket drug spending reached the catastrophic coverage phase of their benefit in 2015 – more than doubling since 2007. Furthermore, the researchers found the share of beneficiaries reaching catastrophic coverage without a low-income subsidy increased considerably, from 18 to 28 percent, between 2007 and 2015. In terms of total Part D expenditures, the portion of Part D expenditures occurring in the catastrophic phase has also significantly increased over the years, from 18 to 37 percent. This is driven in large part by spending from beneficiaries without a low-income subsidy. The researchers estimate that implementing a cap for all Part D enrollees in 2015 would have raised premiums by only one to four percent – amounting to a monthly premium increase of only $0.40- $1.31 per member.
The full study is available at Health Affairs. A press release about the study is available here.
Citation: Trish, E., Xu, J., Joyce, G. (2018). Growing Number of Subsidized Part D Beneficiaries With Catastrophic Spending Suggests Need For An Out-Of-Pocket Cap. Health Affairs.