The U.S. Centers for Disease Control and Prevention (CDC) started recommending protective behaviors such as hand hygiene and social distancing in March 2020 as the COVID-19 pandemic spread globally. In April 2020, the CDC added non-medical mask use.
How protective behaviors were adopted depended in part on the individual’s association of COVID-19 with common infectious diseases. This is according to a new study published in the April 2021 edition of Social Science & Medicine.
Early in the pandemic, COVID-19 was compared to seasonal influenza by elected officials in the United States, perhaps to downplay the need for protective behaviors. Meanwhile, the World Health Organization warned that, despite similarities in symptoms and transmission routes, COVID-19 had greater rates of severe disease and mortality, and no licensed vaccines or therapeutics.
In March 2020, Schaeffer Center expert Wändi Bruine de Bruin and colleagues surveyed 6,534 U.S. adults as part of the Understanding America Study asking them to list diseases that came to mind when thinking of COVID-19. Participants also completed questions that asked about demographics, risk perceptions and protective behaviors.
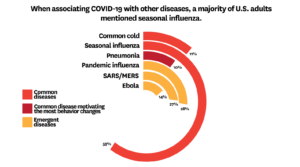
Seasonal influenza (59%) was the most common illness associated with COVID-19 across all demographic groups, according to the analysis. This was followed by pandemic influenza (28%), SARS/MERS (27%), Ebola (14%), common cold (11%) and pneumonia (10%).
The survey data indicated that, with few exceptions, mentioning seasonal influenza or the common cold tended to be associated with lower likelihood of reporting protective behaviors like hand hygiene, social distancing and non-medical mask use. By comparison, mentioning pneumonia or emergent infectious diseases (pandemic influenza, SARS/MERS, and Ebola) was associated with engaging in the most protective behaviors.
For example, 55% of individuals that associated COVID-19 with seasonal flu and 57% of individuals that associated it with the common cold reported that they were avoiding crowds as a protective behavior. In comparison, 62% of individuals associating COVID-19 with pneumonia said they were actively avoiding crowds.
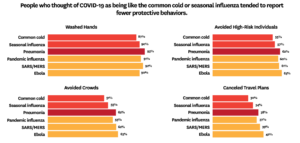
Across participants, 90% indicated washing hands, 57% avoiding public spaces or crowds, 58% avoiding high-risk individuals, and 37% canceling or postponing travel.
When accounting for demographic and risk perceptions, mentioning the common cold was associated with lower likelihood of reporting two of the four protective behaviors. Additionally, mentions of pneumonia, SARS/MERS, and Ebola were associated with greater likelihood of reporting three of the four protective behaviors.
Race was the only demographic variable that showed a significant difference in mentioning each disease. Specifically, relatively more white participants mentioned seasonal influenza and the common cold when associating COVID-19. Black and Latino participants mentioned pneumonia and Ebola while other minority participants mentioned SARS/MERS more.
When faced with a novel, infectious disease, it is widely understood that people try to draw comparisons to other diseases. The findings suggest that those comparisons could have implications for whether or not individuals engage in protective behaviors. To motivate changes in behavior in response to possible future pandemics, public health risk communications may need to mention diseases that resonate with people, while retaining accuracy.
COVID-19 risk communications that aim to promote protective behaviors may be more effective if they avoid drawing comparisons to seasonal influenza or common cold, and instead mention pneumonia, SARS/MERS, or Ebola. Because symptoms of COVID-19 are more similar to those for pneumonia and SARS/MERS than to Ebola, those may be the more appropriate diseases to mention.
The full study is available in the April 2021 edition of Social Science & Medicine.

You must be logged in to post a comment.