USC-led research suggests federal, state and local policymakers should consider targeted strategies to protect access to pharmacies most at risk for closure.
Key findings:
- The rate of pharmacy closures has more than doubled in recent years, with nearly 1 in 3 pharmacies shuttering between 2010 and 2021—contributing to an unprecedented decline in the availability of pharmacies in the United States.
- About one-third of counties experienced an overall decline in pharmacies, and the risk of closure was higher in predominantly Black and Latino neighborhoods.
- Independent pharmacies, often excluded from networks by pharmacy benefit managers, were more than twice as likely to face closure compared to chain pharmacies.
- Policymakers should consider policies to expand pharmacy participation in preferred networks, particularly for Medicaid and Medicare Part D plans.
About 1 in 3 U.S. retail pharmacies have closed since 2010, with the vast majority of states experiencing an overall decline in pharmacies in recent years, according to a new study from researchers at USC and the University of California, Berkeley. Pharmacy closures significantly impact public health by making it harder for people to access prescriptions and essential health services.
The study, published Dec. 3 in the journal Health Affairs, analyzes local and market characteristics of pharmacy closures between 2010 and 2021. With thousands of pharmacy closures expected in the coming years, the researchers’ findings offer a roadmap for identifying which communities are most at risk of losing pharmacies and for crafting policies that may help them survive.
“At the same time many states are making efforts to expand the scope of pharmacy services beyond dispensing drugs to include the provision of preventive and emergency care, we found that there are—for the first time for at least a decade—fewer pharmacies available to provide them,” said senior author Dima Mazen Qato, Hygeia Centennial Chair at USC Mann and a senior scholar at the USC Schaeffer Center for Health Policy & Economics.
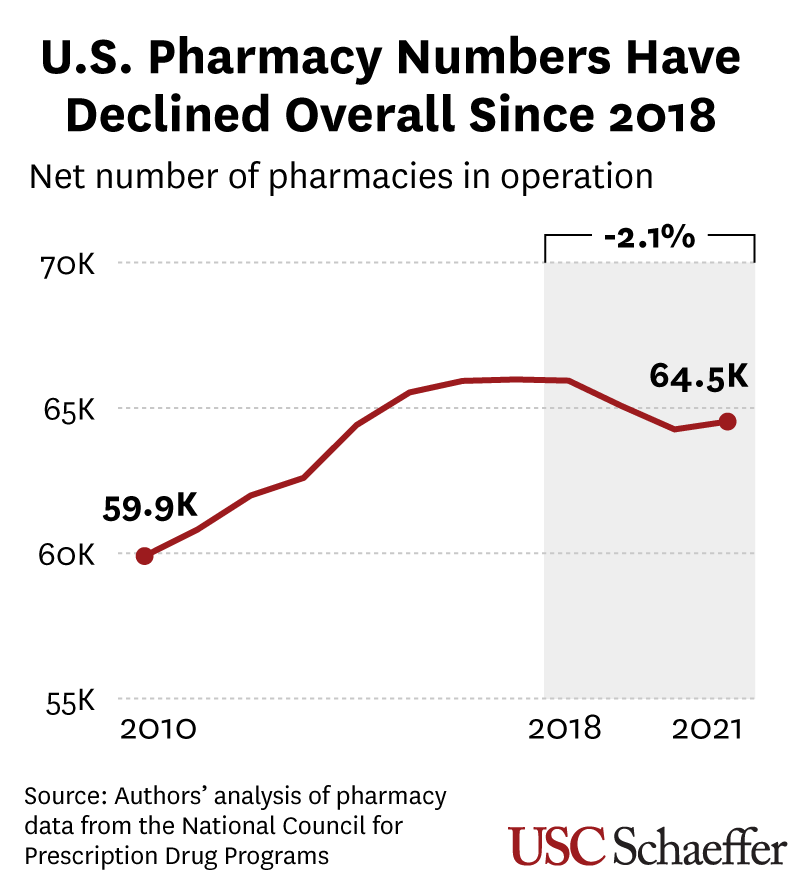
Accelerating closures have led to net loss in pharmacies for the first time since at least 2010
For most of the 2010s, pharmacy openings in the U.S. outpaced closures. In previous work, the researchers found that pharmacies closed at a much slower rate during the first half of the decade, with 1 in 8 drugstores shuttering between 2009 and 2015.
However, their new study reveals an unprecedented decline in the number of pharmacies began in 2018, primarily driven by closures of chain pharmacies during an active period for industry consolidation. This included the merging of large pharmacy chains with dominant pharmacy benefit managers (PBMs), which negotiate prescription drug benefits but also steer patients to preferred pharmacies.
Researchers identified pharmacies using a registry maintained by a national nonprofit and linked the data to county- and neighborhood-level data from the U.S. Census Bureau and the National Center for Health Statistics. Among their findings:
- Between 2018 and 2021, the number of pharmacies declined in 41 states. During the entire study period (2010-2021), nearly one-third of counties experienced a net decline in pharmacies, affecting 91.6 million people.
- In seven states, more than half of counties experienced a net decline in pharmacies: Illinois, Maine, Mississippi, New York, Pennsylvania, Rhode Island and Vermont.
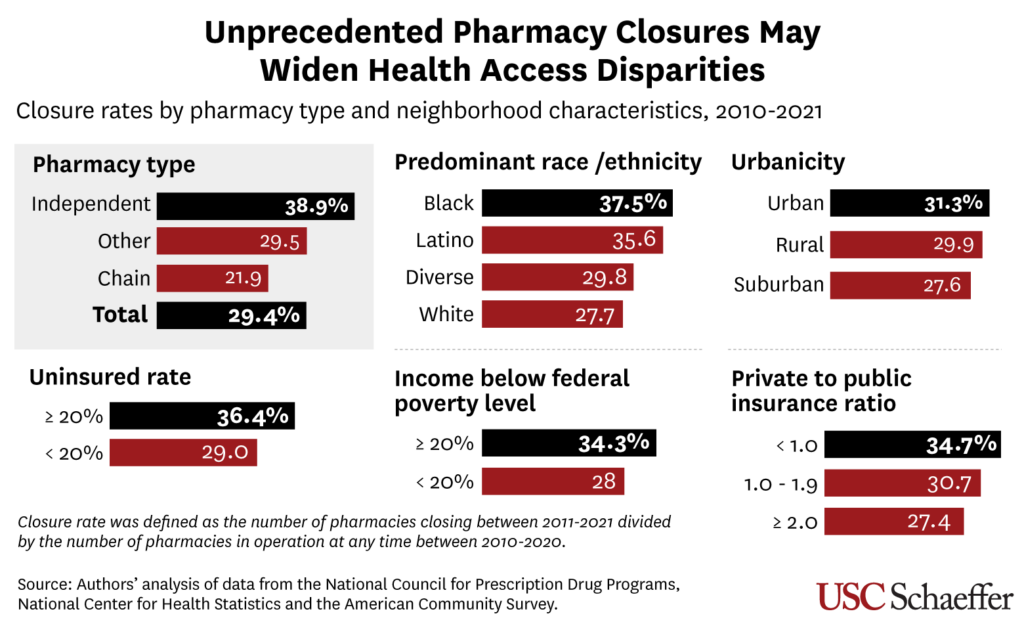
- At the community level, pharmacy closure rates were higher in predominantly Black and Latino neighborhoods—37.5% and 35.6%, respectively—than predominately white ones (27.7%).
That last finding is partly explained by the struggles of independent pharmacies, which were more than twice as likely to close as chain stores. They were also much more likely to be in Black, Latino and low-income neighborhoods, as well as those with disproportionate rates of people with Medicare or Medicaid coverage.
“Our findings suggest that closures may widen health disparities in access to prescription and other essential pharmacy services, such as vaccinations and pharmacist-prescribed regimens, including contraceptives, medications for HIV prevention, and treatments for opioid use disorder,” said first author Jenny Guadamuz, assistant professor at the UC Berkeley School of Public Health and Health Equity Program director for the UC-Berkeley Center for Health Management & Policy Research.
“Without safeguarding pharmacies in marginalized neighborhoods, expanding health care services at pharmacies may enhance convenience for more affluent populations while failing to address the health needs of communities disproportionately affected by pharmacy closures, particularly Black and Brown populations in low-income urban areas,” Guadamuz added.
Preventing Future Closures
“As highlighted in a recent FTC report, a key factor contributing to the higher risk of closure for independent pharmacies may be their frequent exclusion from preferred pharmacy networks,” Guadamuz said. PBMs use preferred pharmacy networks to encourage patients to visit certain locations by offering lower cost-sharing or out-of-pocket costs. The recent mergers of large pharmacy chains and PBMs also likely contributed to low reimbursements from PBMs at these combined companies to independent pharmacies and rival chain pharmacies, the researchers noted.
The researchers urge federal and state policymakers to consider policies that would increase participation of independent pharmacies in preferred networks. This could include mandating Medicare and Medicaid plans to give preferred status to pharmacies at heightened risk of closure or those serving “pharmacy deserts” with reduced access to pharmacy services.
In the commercial market, federal and state regulators should also consider requiring that PBMs’ preferred networks do not disproportionately favor pharmacy chains, including those part of the same company, the researchers said.
“Federal, state and local policies and programs should consider targeted strategies, including increases in Medicare Part D and Medicaid pharmacy reimbursement rates, to protect critical access to pharmacies most at-risk for closure, particularly those serving neighborhoods that are or are at risk of becoming pharmacy deserts,” Qato noted.
About This Study
Other authors include Genevieve Kanter of USC and G. Caleb Alexander of Johns Hopkins University.
Support for this research was provided by the National Institute on Aging, National Institutes of Health (Grant No. R01AG080090-01). The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Sign up for Schaeffer Center news


You must be logged in to post a comment.