Specialty drugs offer substantial benefits to a select group of people with complicated drug and medical needs but they come with very high price tags. Solvaldi, a specialty drug used to treat Hepatitis C, came under public scrutiny for its high price of $1,000 a day (or $84,000 for a full course of treatment). These drugs are used to treat complex medical conditions such as rheumatoid arthritis, multiple sclerosis, and cancer. Though there prices draw public criticism, the drugs are priceless for those who could truly benefit from them.
Thus, the escalating price of drugs and health care raises concern about access and out-of-pocket costs for patients, especially those who could benefit from the treatment options of specialty drugs. According to a recent study published in Health Affairs by Schaeffer Center researchers Erin Trish, Geoffrey Joyce, and Dana Goldman, annual specialty drug spending for Medicare beneficiaries who use these types of pharmaceuticals increased more than threefold between 2007 and 2011, from $2,641 to $8,976.
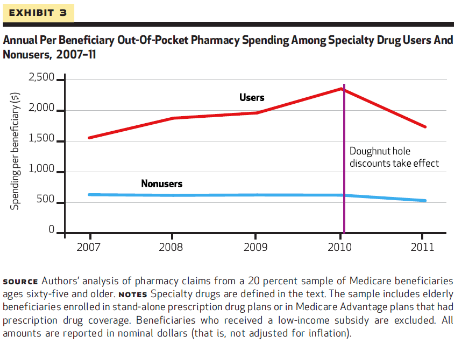
Trish and her coauthors compared the growth in the contribution of specialty drug spending to overall general drug spending. The authors found that although annual specialty drug spending has increased substantially for patients using the drugs since 2007 (see exhibit), yet there has been a 26% reduction in out-of-pocket spending for these patients recently.
The authors attribute this drop in spending to ACA provisions that changed the cost sharing designations for beneficiaries experiencing the doughnut hole- the gap in coverage in the Medicare Part D plans.
It is clear that the benefit of specialty drugs for the population who needs them is substantial. Reducing coverage, as has been proposed by some, would negatively impact the overall well-being of individuals in this population as well as add a significant cost burden.
Specialty drug pricing trends in Medicare with regards to moving designations from Part B medical benefit to Part D pharmacy benefit has likely played an important role in the cost burden, according to the researchers. Policymakers will need to keep these trends in mind as the debates over healthcare costs and Medicare continue.