Editor’s Note: This analysis is part of the USC-Brookings Schaeffer Initiative for Health Policy, which is a partnership between Economic Studies at Brookings and the University of Southern California Schaeffer Center for Health Policy & Economics. The Initiative aims to inform the national healthcare debate with rigorous, evidence-based analysis leading to practical recommendations using the collaborative strengths of USC and Brookings.
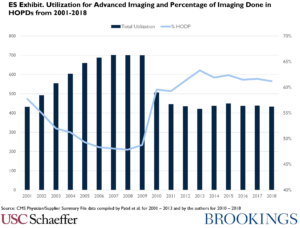
Medicare’s experience of paying for outpatient imaging services, particularly expensive advanced imaging such as MRIs, CAT scans, and nuclear scans, has been tumultuous over the last 20 years. The period was characterized by substantial increases in performance of advanced imaging services, mainly in doctors’ offices, followed by a shift to hospital outpatient departments (HOPDs) and then a leveling off of utilization, as shown in the chart below. These trends were influenced by an extraordinary number of legislative and regulatory policy changes, most of which reduced payment amounts for services paid under the Physician Fee Schedule (PFS) in doctors’ offices. This likely contributed to a movement of services to HOPDs, with payment based on the Outpatient Prospective Payment System (OPPS) where rates have been less impacted by policy changes. We termed this policy making process “dysfunctional” because there is no evidence that the results were anticipated or planned, despite the dramatic effect they have had on where advanced imaging is performed and at what cost. Moreover, we are not convinced that the current policy direction will result in a more coordinated and strategic approach.
Despite the recent leveling of the volume of advanced imaging per 1,000 Medicare beneficiaries, both the price and utilization are considerably higher in the US than in other developed countries. In addition, the fee schedule payment amounts have evolved over the study period such that the payments for the same high-volume services are consistently higher in the OPPS than in the PFS. This phenomenon contributes to the trend of hospital acquisition of physician practices, a development that undermines competition in the physician and hospital services markets.
We offer three recommendations for improving Medicare’s treatment of advanced imaging in ambulatory settings, two of which focus on setting prices and one on managing utilization.
- First, CMS needs a more systematic method of establishing payment levels for services using expensive equipment involved in the performance of advanced imaging studies. Surveys conducted to obtain such data in the past have not been repeated and current data are lacking. While calls for better data are commonplace in critiques of Medicare payment, advanced imaging is one area where equipment is the dominant component of costs and changes rapidly as technology advances.
- Second, CMS should coordinate the process for setting payments under the PFS and OPPS. Historically, setting payments for advanced imaging that can be performed in either HOPDs or physician offices have been independent of one another, resulting in often widely diverging fees and shifts in site of care to take advantage of payment differences. Site neutrality should guide the process. Recognizing that hospitals will have higher overhead costs due to the need for 24/7 staffing for emergency patients and inpatient needs, a modest differential in rates would be justified, but we believe that it should not be as large as current differentials.
- Third, we believe that prior authorization, a system widely used by private insurers to control spending for advanced imaging and other expensive services, should be used to manage advanced imaging services paid under the PFS and OPPS. Prior authorization requires providers to seek permission to perform an advanced imaging study for the service to be covered, but it can be used selectively by excusing the requirement for those physicians with acceptable patterns of use. Medicare is instead embarking on a system called Appropriate Utilization Controls (AUCs), which relies on decision-support mechanisms but has not been used as a payment tool. While the law establishing the AUC program allows for prior authorization to be called upon in cases where clinicians are shown to be outliers in their ordering of advanced imaging, CMS has not provided information on how outliers will be identified and how prior authorization will be applied. We hope that CMS will draw on the vast experience of private insurers and elevate prior authorization from a secondary to a primary tool to manage advanced imaging if the AUC program proves to be unduly permissive.
Disclosures: The authors did not receive financial support from any firm or person for this article or from any firm or person with a financial or political interest in this article. They are currently not an officer, director, or board member of any organization with an interest in this article.

You must be logged in to post a comment.