Objectives
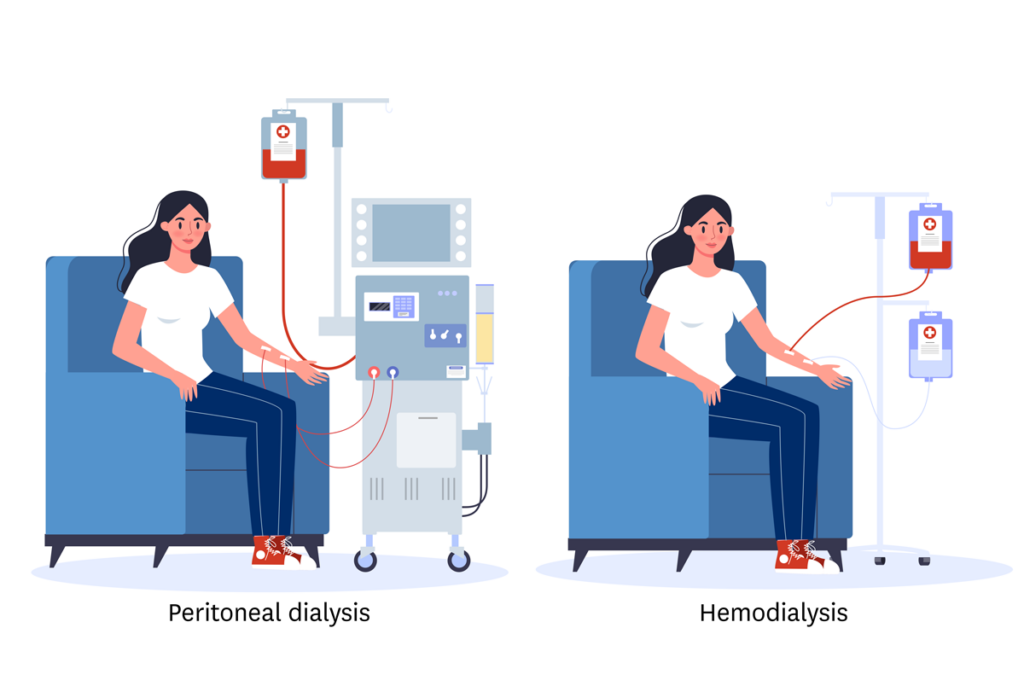
Policy makers have suggested increasing peritoneal dialysis (PD) would improve end-stage kidney disease (ESKD) outcomes and reduce Medicare spending compared with hemodialysis (HD). We compared mortality, hospitalizations, and Medicare spending between PD and HD among uninsured adults with incident ESKD.
Methods
Using an instrumental variable design, we exploited a natural experiment encouraging PD among the uninsured. Uninsured patients usually receive Medicare at dialysis month 4. For those initiating PD, Medicare covers the first 3 dialysis months, including predialysis services in the calendar month when dialysis started. Starting dialysis later in a calendar month increases predialysis coverage that is essential for PD catheter placements. The policy encourages PD incrementally when ESKD develops later in the month. Dialysis start day appears to be unrelated to patient characteristics and effectively “randomizes patients” to dialysis modality, mitigating selection bias.
Results
Starting dialysis later in the month was associated with an increased PD uptake: every week later in the month was associated with an absolute increase of 0.8% (95% confidence interval [CI] 0.6%-0.9%) at dialysis day 1 and 0.5% (95% CI 0.3%-0.7%) at dialysis month 12. We observed no significant absolute difference between PD and HD for 12-month mortality (−0.9%, 95% CI −3.3% to 0.8%), hospitalizations during months 7 to 12 (−0.05, 95% CI −0.20 to 0.07), and Medicare spending during months 7 to 12 (−$702, 95% CI −$4004 to $2909).
Conclusions
In an instrumental variable analysis, PD did not result in improved outcomes or lower costs than HD.
The full study is available in ScienceDirect.