The USC-Brookings Schaeffer Initiative for Health Policy aims to produce high-quality, high-impact research and develop innovative policy solutions to the most pressing health care challenges. During the COVID-19 pandemic, the Initiative’s work and expertise have been valuable to policymakers trying to address the COVID crisis and those seeking to understand new laws mandating free coverage of testing and vaccines, economic relief packages, and how to navigate choosing a health plan after losing job-based coverage. The global pandemic showcased the important work of the Initiative in addressing immediate needs for data-driven research as policymakers strive to meet the challenges posed by the COVID crisis.
Paul Ginsburg, Director of Public Policy at the USC Schaeffer Center for Health Policy & Economics and the Leonard D. Schaeffer Chair in Economic Studies at Brookings, leads the Initiative, working closely with Loren Adler, Initiative Associate Director, and Dana Goldman, Director of the USC Schaeffer Center for Health Policy & Economics.
Explore Schaeffer Initiative Research ↓

“Despite the challenges of a pandemic, the Schaeffer Initiative was able to leave its evidence-based imprint on federal policy. We owe much of that success to Paul Ginsburg’s expert leadership navigating a divided government.”
Dana Goldman, Director, USC Schaeffer Center for Health Policy

The USC-Brookings Schaeffer Initiative for Health Policy, now in its sixth year, provides timely and compelling health policy research and rigorous analysis, bringing together expertise from across the country. As 2020 presented new challenges brought on by the COVID pandemic, the Initiative shifted to virtual research and events on the pressing health policy issues facing the nation.
The Initiative benefits from the strengths of both the Economic Studies program at Brookings and the USC Schaeffer Center, producing data-directed health policy analysis with cogent recommendations for policy. By collaborating coast to coast, our unique team of scholars work to highlight and encourage meaningful reforms and policy solutions to help lower health care prices and strengthen the U.S. health care system.
The USC-Brookings Schaeffer Initiative focused in 2020 on four main areas:
- The COVID-19 Crisis
- Regulatory and Legal Challenges to the Affordable Care Act
- Surprise Medical Bills
- The Future of Health Care Reform
The Initiative publishes white papers that probe dense health policy problems and shorter timely analyses of pressing proposals, in addition to developing new policy proposals, all with an eye toward informing policymakers. The Initiative also holds public conferences, held remotely as webinars throughout 2020, and private briefings to help foster communication and engagement among policymakers and other stakeholders from both the private and public sectors.


Schaeffer Initiative experts proved a vital resource to policymakers and media on questions concerning the COVID-19 pandemic and the eventual health care landscape post-pandemic. Schaeffer Initiative experts frequently engaged with policymakers in the administration, Congress, and states; provided testimony and commentary, recommendations and technical assistance; and spoke frequently regarding the impact of COVID-19, surprise billing, and the Affordable Care Act.
As in previous years, the Initiative continues to serve as a key resource for understanding policy solutions to surprise out-of-network medical billing and prescription drug pricing and coverage. Initiative experts also analyzed options to regulate health care prices, expand coverage, and curtail substandard health insurance plans that leave beneficiaries vulnerable to catastrophic financial risk.
Congressional and Administration Interaction
Schaeffer Initiative scholars are frequently sought after by Congress and the White House as experts across several policy areas. Over the past year:
“Anybody who has been serious about operationalizing auto-enrollment (health insurance) at any meaningful scale is thinking about changing our eligibility rules. It’s not possible to tackle this policy problem without reimagining the way we do eligibility — to make it more stable and more predictable over time. And that’s coming from the left and from the right.”
Christen Linke Young in Schaeffer Initiative webinar, “Health Insurance Auto-Enrollment” (May 18, 2020)
- Paul Ginsburg serves as Vice Chair of the Medicare Payment Advisory Commission, which advise both the Congress and the Center for Medicare and Medicaid Services (CMS) on a wide range of Medicare payment issues.
- Dana Goldman provided insights to Health and Human Services, CMS, the Food and Drug Administration, the White House, and multiple Congressional members on a range of topics including drug rebates, Alzheimer’s treatment, insulin pricing, and COVID-19 forecasts.
- Matthew Fiedler responded to inquiries from the staffs of multiple Congressional committees and multiple members of Congress across both houses on a range of topics, including the fiscal policy response to COVID-19, approaches to reducing provider prices, and options to improve the Affordable Care Act’s subsidy structure.
- Matthew Fiedler served on the Congressional Budget Office’s technical review panel for its health insurance microsimulation model.
- Matthew Fiedler provided comments on drafts of reports issued by the Congressional Budget Office and the Medicare Payment Advisory Commission.
- Loren Adler and Christen Linke Young briefed a bipartisan group of 11 members of the House of Representatives on surprise billing.
- At the request of Committee staff, Loren Adler provided advice on federal policy to support COVID-19 testing efforts and guardrails to place on the CARES Act’s Provider Relief Fund.
- Loren Adler provided technical assistance to staff from multiple Committees on surprise billing and the role of private equity.
- Recommendations on how to enable novel pricing strategies for drugs from a 2017 Schaeffer Initiative paper by Darius Lakdawalla, Rachel Sachs, and Nicholas Bagley were implemented by CMS.
- The FDA cited the work of Darius Lakdawalla, Dana Goldman, and Erin Trish on the use of pooled testing as an efficient way to get people back to work and students back to school.
- Erin Trish discussed insulin pricing, out-of-pocket spending, and Medicare Part D reforms with CMS Administrator Seema Verma and staff from CMMI, Council of Economic Advisors, National Economic Council, Domestic Policy Council, Office of Management and Budget, Office of American Innovation, and Speaker Nancy Pelosi’s office.
- Christen Linke Young spoke with Congresswoman Blunt Rochester’s office regarding auto-enrollment.
- Christen Linke Young spoke with Senate Aging Committee staff regarding junk insurance.
- Christen Linke Young spoke frequently with the House Committee on Energy and Commerce, the House Committee on Education and Labor, and the Ways and Means Committee regarding the COVID response.
- Christen Linke Young discussed improvements to the Affordable Care Act with staff from Senator Mark Warner’s office.
- House Committee on Energy and Commerce released a report on short-term plans that cited Kathleen Hannick and Christen Linke Young’s paper on COVID and junk insurance plans.
- Christen Linke Young had conversations with House Committee on Energy and Commerce and the House Committee on Education and Labor staff on fixed indemnity coverage and potential pathways for oversight. The House Committee on Education and Labor subsequently sent a letter to the Department of Labor on the use.
- Christen Linke Young had a conversation with a federal contractor preparing a report for CMS on issues related to verification of eligibility for coverage programs.
- Christen Linke Young spoke with Congressman Lloyd Doggett’s staff regarding denials of prior approval.
- In November, Christen Linke Young took a leave of absence to serve on the Biden transition team.
- Neeraj Sood presented findings on the pharmaceutical distribution system to the Department of Justice Antitrust Division.
- Neeraj Sood and Karen Van Nuys discussed their findings on the pharmaceutical distribution system with staff from multiple Congressional offices, the Council of Economic Advisors, and the Senate Finance Committee.
State and Local Lawmaker Interaction
- Loren Adler provided technical assistance to state leaders in Indiana, Maine, and Virginia in crafting surprise billing legislation that passed in 2020. Along with Matthew Fiedler, Paul Ginsburg, and Christen Linke Young, Adler penned and organized a large bipartisan sign-on letter sent to legislative leadership in Indiana, which explained the virtues of the so-called network matching approach to eliminating surprise billing. This group also discussed surprise billing with the state’s Department of Insurance. Indiana ended up passing a similar approach, the first state law that will protect patients enrolled in self-insured employer health plans.
- Christen Linke Young discussed junk health insurance plans with the New York State Department of Financial Services.
- Christen Linke Young had conversations with the Department of Insurance in Kentucky and New Mexico regarding connecting unemployment insurance application systems to coverage.
- Christen Linke Young had a conversation with Covered California on a state auto-enrollment proposal.
- Neeraj Sood presented on pharmacy benefit managers to the Wisconsin Governor’s task force on reducing prescription drug costs and to the California Department of Managed Care.
- In partnership with the Los Angeles County Department of Health, Neeraj Sood developed a testing strategy for COVID-19.
- Neeraj Sood presented on the pharmaceutical distribution system to the Oregon Task Force on Fair Pricing of Prescription Drugs and to the California PBM Task Force.
Influential Committee Appointments
- Paul Ginsburg serves on the National Academies’ Committee on Emerging Science, Technology and Innovation in health and medicine.
- Paul Ginsburg serves on the Advisory Board of the National Institute for Health Care Management.
- Paul Ginsburg serves as a member of the Aspen Health Strategy Group, which is preparing a report on maternal mortality in the United States.
- Darius Lakdawalla serves on Addressing Sickle Cell Disease: A Strategic Plan and Blueprint for Action, National Academies of Sciences, Engineering and Medicine.
- Neeraj Sood serves on Committee on the Prevention and Control of Sexually Transmitted Infections in the United States, National Academies of Sciences, Engineering and Medicine.
The Essential Scan
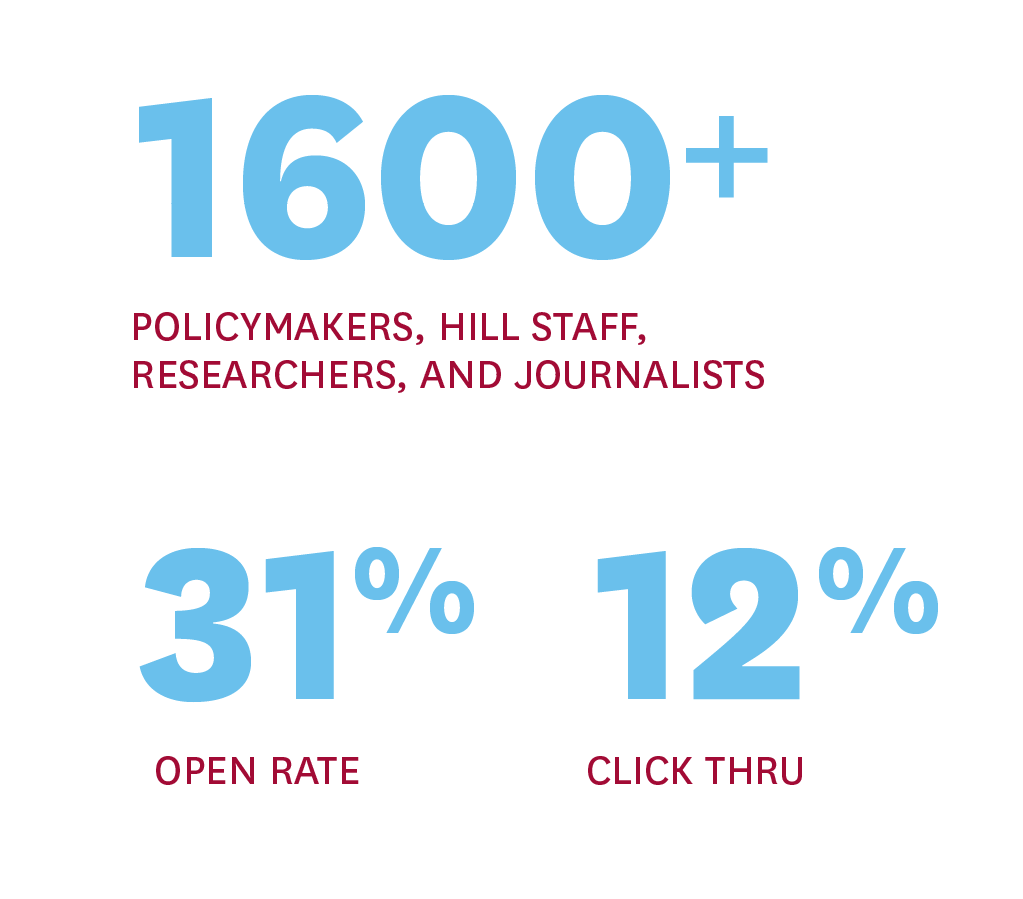
The Essential Scan, a biweekly email newsletter produced by the Initiative, highlights new research with significant health policy implications, especially research on topics that the Initiative scholars work on. The publication is sent to a growing list of over 1,600 policymakers, Hill staff, researchers, and journalists, and consistently receives a high open rate of 31 percent and a click through rate of 12 percent.

“So these viruses are out there. What can we do? We can do the equivalent on a bigger scale for what we’ve done for bioterrorism. After the anthrax attack just following 9/11, we set up a government-run machinery to approach the problem of how to protect ourselves from bioterrorism.”
William Haseltine in Schaeffer Initiative webinar, “A Short and Long-term Approach to COVID-19” (April 17, 2020)
The United States health care system has been under unprecedented pressure during the worldwide pandemic. Relief legislation, Administration initiatives, and evolving policies aim to protect the newly uninsured, encourage people to get tested, and spur vaccine development, as well as prevent excessive billing for those who are infected with the virus and seek treatment. The Initiative has been at the forefront of these changes, working to clarify new policies and present new research and analysis to improve future strategies. The Initiative team published multiple pieces this year addressing various issues related to the COVID-19 pandemic response and will continue to produce blogs and more extensive reports analyzing and critiquing policies.
The Initiative hosted a webinar in April, “A Short and Long-term Approach to COVID-19,” with Paul Ginsburg in conversation with William Haseltine, a renowned expert in the field of infectious diseases and genomics. They discussed the importance of testing, contact tracing, and controlled quarantine to help track cases and reduce transmission over time.
Initiative fellows were sought after as experts on the COVID-19 response. Loren Adler, Dana Goldman, Christen Linke Young, Matthew Fiedler, Erin Trish, Neeraj Sood, and Paul Ginsburg frequently provided briefings and technical assistance to several Congressional offices, the Administration, and to individual states and counties. Additionally, they were widely interviewed and quoted in the media for their work, including in The New York Times, The Washington Post, NPR, and Politico, among other outlets.
Initiative scholars penned multiple articles analyzing policies to cover the costs of COVID-19 testing and suggesting ways to expand testing. In April, Loren Adler published an explanation of how the CARES Act would affect COVID-19 test pricing, and then in July, he co-authored with Christen Linke Young a deep dive into the laws governing COVID-19 test payment and how to improve them. Together, these two blogs have been viewed over 45,000 times.

Neeraj Sood worked closely with the Los Angeles County Department of Public Health in the development of testing strategies that use rapid COVID-19 tests. Sood’s opinion piece in The Wall Street Journal in March noted the importance of expanding testing efforts beyond individuals with symptoms. The FDA cited a Schaeffer Center white paper on pooled testing by Darius Lakdawalla, Dana Goldman, Emmet Keeler and Erin Trish. Lakdawalla and Goldman penned a piece in The Hill suggesting pooled testing as a way to get Americans back to work and school. The white paper and related opinion pieces had over 67,000 views.
Initiative scholars also published two blogs in Health Affairs related to COVID-19 as part of larger collaborations. In early March, Kavita Patel and Christen Linke Young, along with a dozen other analysts, produced a blog, “Health Care Priorities for a COVID-19 Stimulus Bill: Recommendations to the Administration, Congress, and other Federal, State and Local Leaders from Public Health, Medical Policy and Legal Experts.” This blog outlined priorities for the stimulus bill including affordable and accessible testing and treatment, specific protections for vulnerable populations including health care workers, as well as enhancing health care delivery, protecting health infrastructure, and, of course, a vaccine. In mid-April, Christen Linke Young and Loren Adler produced a second blog, “Responding to COVID-19: Using the CARES Act’s Hospital Fund to Help the Uninsured, Achieve other Goals.” This piece highlights the protections in the initial $100 billion provider relief fund, how to utilize the funding to support the uninsured, and how to help alleviate the significant financial and logistical challenges hospitals are reckoning with.
Neeraj Sood and colleagues authored a study in November 2020 examining the unprecedented strain on patients, health care professionals, and institutions caused by COVID-19. Published by JAMA Open Network, the new study found that overall healthcare use declined by 23% in March 2020 and 52% in April 2020 with drops in diagnostic procedures unable to be conducted by telemedicine especially precipitous. In March and April, colonoscopies decreased by nearly 70% when compared to the same period in 2019. Meanwhile, reductions in mammograms were 67% among women age 46 to 64. The researchers also found race and income disparities at the zip code level exist in telemedicine use.
In late April, Matthew Fiedler published an opinion piece in The New York Times, titled “States Are Being Crushed by the Coronavirus. Only This Can Help,” outlining the immense fiscal pressure state governments would face due to the economic damage caused by the pandemic and the costs of leading their individual COVID-19 responses. The piece detailed the amount of fiscal relief states would need to stave off the cascading economic damage done if states cut spending in response to budget shortfalls.

The Affordable Care Act has been hotly debated this year nation-wide
as well as in several statewide court deliberations. Initiative Fellows published two pieces in Health Affairs and another in JAMA. In “The ACA’s Individual Mandate In Retrospect: What Did It Do, And Where Do We Go From Here” for Health Affairs, Matthew Fiedler examined recent analysis on the mandate’s effects and how to further expand coverage in a cost-effective manner. Working with Aviva Aron-Dine, Christen Linke Young published “Silver-Loading Likely to Continue following Federal Circuit Decision on CSRs” in Health Affairs that outlined the consequences of the Court’s decision to allow insurers to recover unpaid cost-sharing reduction payments, and what the future guidance on silver loading should include.

Matthew Fiedler, Loren Adler, and Christen Linke Young also published “Health Care in President Trump’s Fiscal Year 2021 Budget” in JAMA, highlighting the Trump Administrations proposed cuts to ACA coverage programs. In addition, Fiedler responded to inquiries from the staffs of multiple Congressional committees and multiple members of Congress across both houses regarding options to improve the Affordable Care Act’s subsidy structure.
Christen Linke Young and Initiative Nonresident Fellow Jason Levitis provided analysis on the Texas v. US lawsuit after it was remanded back to lower courts, extending the period of uncertainty for Texans and damaging all stakeholders across the health care industry. In addition, Young and Levitis produced multiple reports on Georgia’s 1332 waiver, in which Georgia policymakers are now pursuing their third attempt to make major changes to the way Georgians access affordable health insurance, including eliminating the Health Insurance Marketplace altogether. They submitted a comment letter to the U.S. Department of Health and Human Services (HHS) the U.S. Department of the Treasury, outlining the ways in which the proposal violates Medicaid rules, the coverage guardrails, multiple Affordable Care Act requirements, and would cause tens of thousands of Georgians to lose coverage. Young and Levitis also submitted a comment letter to HHS regarding the Notice of Benefit and Payment Parameters for 2021 (CMSD-9916-P), arguing that the agency’s attempts to change the Advance Premium Tax Credit are both unlawful and exceed their authority.
Throughout 2020, Christen Linke Young worked to detail the myriad forms of junk insurance available, including some encouraged by the Trump Administration, and elucidate regulatory and legislative options to curtail these plans. She produced an expansive white paper that provides an in-depth analysis of health plans that do not meet quality standards, meaning they do not cover a comprehensive array of health care services or have a design that ensures consumers bear only a reasonable share of the cost. She also penned a blog outlining the dangers of fixed indemnity health coverage, how they manage to squeeze through a wide variety of loopholes, and how they take advantage of beneficiaries through problematic and nontransparent ways. Young discussed pathways to regulation and oversight on these plans with staff from multiple Congressional Committees and state insurance departments. And finally, The House Committee on Energy and Commerce released a report on short-term plans that cites Kathleen Hannick and Christen Linke Young’s paper on COVID-19 and junk insurance plans.
The pandemic also exacerbated the need to help the newly unemployed find health insurance coverage. Christen Linke Young and Sobin Lee produced a report, “Making ACA Enrollment More Automatic for the Newly Unemployed,” and Young worked with insurance departments in Kentucky and New Mexico to help connect unemployment insurance application systems to health coverage.
The study revealed that education has an outsized impact on the prospects of people with severe mental disorders.

“The No Surprises Act, while imperfect, represents a significant win for consumers that will put an end to nearly all surprise bills and should modestly reduce premiums. Schaeffer Initiative experts will now turn to making sure implementation goes smoothly so that the law achieves its objectives.”
Loren Adler, Associate Director, USC-Brookings Schaeffer Initiative for Health Policy
The No Surprises Act, enacted at the end of 2020, marks the culmination of years of effort, making illegal nearly all surprise out-of-network billing across the nation. Schaeffer Initiative experts were involved every step of the way, from its first report on the topic in 2016, to white papers and journal articles that defined the market failure and detailed solutions, to leading dozens of Congressional briefings for staff and members who frequently called on Initiative experts for technical assistance.
In the legislation, lawmakers steered clear of the approaches taken by New York and New Jersey that Initiative experts demonstrated could perversely increase health care prices. The new law is expected to both end surprise bills and modestly reduce insurance premiums.
The Initiative released five publications on surprise billing in the past year focusing on state laws, surprise bills from air ambulances, and how policies to address surprise billing could lower premiums for all. Christen Linke Young and Loren Adler regularly provided assistance to Congress, the Administration, and individual states. Adler provided technical assistance to state leaders in Indiana, Maine, and Virginia in crafting surprise billing legislation that passed in 2020. Adler also penned and organized a large bipartisan sign-on letter sent to legislative leadership in Indiana, along with Paul Ginsburg, Matthew Fiedler, and Young, which explained the virtues of the so-called network matching approach to eliminating surprise billing. Indiana ended up passing a similar approach, the first state law that will protect patients enrolled in self-insured employer health plans.
Additionally, in one of the few in-person interactions of 2020 (in February), Adler and Young briefed a bipartisan group of 11 members of the House of Representatives on surprise billing.

Erin Duffy, Loren Adler, Paul Ginsburg, and Erin Trish published a piece in Health Affairs analyzing the prevalence and characteristics of surprise out-of-network bills in ambulatory surgery centers. This piece outlined the rapid increases in costly surprise bills and emphasized the need for federal policy to expand protections for all patients. Erin Trish, Bich Ly, Mark Hall, Adler, and Erin Fuse Brown also published a report in The Milbank Quarterly analyzing the prevalence, magnitude, and policy solutions for out-of-network air ambulance bills. The report estimated more than three-quarters of air ambulances are out-of-network and found two-in-five transports resulted in a potential balance bill. Adler, Kathleen Hannick, and Sobin Lee penned a blog reporting on the concentration of high air ambulance charges in private equity-owned carriers and outlined policy solutions to allay mounting prices.
In addition to focusing on out-of-network air ambulance bills, Initiative scholars examined the impact of surprise medical bills on premiums for patients who do not receive a surprise bill. Erin Duffy, Bich Ly, Loren Adler, and Erin Trish estimated that policies to address surprise billing could reduce health insurance premiums by 1% to 5%, in addition to protecting patients from receiving costly, unexpected bills. These projected savings could reduce premiums for the nation’s commercially insured population by roughly $12 billion to $39 billion, respectively. This piece was published in The American Journal of Managed Care.
Two more papers have been accepted and are scheduled for publication in 2021 – one investigating the unique features of anesthesia payment and another analyzing the outcomes of arbitration over surprise bills in New Jersey – in the American Journal of Managed Care and Health Affairs, respectively.


“Thankfully, unlike many problems spawned by COVID-19, the coming state budget crisis has a straightforward solution: The federal government can borrow freely and currently at very low interest rates, so it can step in and offer aid to states. … One particularly good approach would be to offer states aid that adjusts automatically based on economic conditions.”
Matthew Fiedler in The New York Times (April 22, 2020)
The Schaeffer Initiative provided research on a diverse range of health policy issues this year with continuing work on prescription drug pricing and coverage, high provider prices, all-payer claims databases, dialysis markets, and auto-enrollment. To inform the fast-moving provider pricing debate, fellows provided several analyses and recommendations for the future of health care policy—how to best control high prices, expand insurance enrollment, and improve the quality of care.
Prescription Drug Pricing and Cost Sharing
The Initiative continues to expand its work on drug policy and innovation, hosting a roundtable of experts in June to discuss effects that price regulation might have on new drug development. The roundtable surfaced insight into the considerations necessary to balance lower prices with incentives for innovation. Steven M. Lieberman, Paul B. Ginsburg, and Kavita Patel published a two-part blog in Health Affairs citing the most prominent takeaways and recommendations for the future. Work led by Dana Goldman and Darius Lakdawalla was foundational to President Trump’s executive order, “Lowering Drug Prices by Putting America First” issued in September. The work showed that between 64% and 78% of worldwide pharmaceutical profits are made from the US and that encouraging other wealthy nations to shoulder more of the burden of drug discovery would ultimately benefit the entire world.
In September, the Initiative hosted a webinar on the policy challenges associated with providing access to hopeful imminent new treatments and diagnostics for Alzheimer’s disease. Leonard Schaeffer opened the event followed by Paul Asien discussing clinical advances and Darius Lakdawalla presenting on payment approaches. Dana Goldman amplified the event discussion in a LinkedIn post.
Throughout the year, Initiative scholars evaluated pharmaceutical pricing and explored how to share rebates with Medicare Part D patients. The Initiative recently completed a grant from The Commonwealth Fund to study Medicare prescription drug payment and rebate reforms. Paul Ginsburg, Steven Lieberman and Erin Trish authored a Health Affairs Blog titled “Sharing Rebates with Medicare Part D Patients: Why and How.” Trish, Geoffrey Joyce, and colleagues published a study in the Schaeffer Center white paper series finding that 20% of Part D beneficiaries would save more than $100 per year if rebates were applied at the point of sale. Karen Van Nuys, Neeraj Sood, and colleagues published a study in the Schaeffer Center white paper series correlating drug rebates and list prices. Their research found that on average a $1 increase in rebates is associated with a $1.17 increase in list price.
Dissecting the House Democrats’ drug price negotiation bill, Paul Ginsburg and Steven Lieberman penned “The Elijah E. Cummings Lower Drug Costs Now Act: How it would work, how it would affect prices, and what the challenges are” for publication on The Commonwealth Fund website.
Addressing High Provider Prices
With high provider prices front and center on the policy stage this year, Matthew Fiedler published a white paper analyzing and modeling the various policy approaches to reducing provider prices. Fiedler offers four possible ways of expanding the public role: capping prices for out-of-network services, capping prices for both in- and out-of-network services, a “default contract” approach, and creating a public option. The report, “Capping prices or creating a public option: How would they change what we pay for health care?” comes after a 3-part series on health care price regulations honoring the late Uwe Reinhardt. The Initiative received a grant from the Robert Wood Johnson Foundation to conduct the virtual webinar series, attracting a live, virtual audience of over 3,300 viewers. Matthew Fiedler also served on the Congressional Budget Office’s technical review panel for its health insurance microsimulation model and provided comments on drafts of reports issued by the Congressional Budget Office and the Medicare Payment Advisory Commission.
Auto-Enrollment
Christen Linke Young continued to explore the possibility of auto-enrollment in the white paper, How Well Could Tax-based Auto-enrollment Work?. The paper outlines the ways in which current health insurance enrollment fails to account for individuals who become uninsured halfway through the year and those who were previously uninsured who gain coverage. This white paper addresses these challenges and proposes retroactive enrollment by utilizing a tax-based auto-enrollment policy. Following its release, the Initiative co-hosted a webinar with the American Enterprise Institute to discuss pathways to automatic enrollment in order to expand quality health insurance coverage. Paul Ginsburg moderated and Young served as a panelist. The webinar had over 1,300 live views. Young’s expertise and insight led to conversations with many Congressional offices concerning auto-enrollment. She also discussed a state auto-enrollment proposal with Covered California.
All-Payer Claims Databases
All-payer claims databases provide important data that could be used to improve policy, share lessons across state lines, and save money. Matthew Fiedler and Christen Linke Young, with funding from The Commonwealth Fund, completed research and provided policy recommendations around the construction of all-payer claims databases. This white paper examines the limitations of today’s all-payer claims databases and the impact of the 2016 Supreme Court Decision, Gobeille v. Liberty Mutual Insurance Co. This decision prohibited states from requiring data collection from non-governmental self-insured group health plans, which represent nearly 61% of enrollment in employer coverage. Fiedler and Young outline several regulatory and legislative options federal policymakers can use to address these limitations to improve all-payer claims database in the future, including creating a national all-payer claims database.
Improving the Dialysis Market
In response to the “Advancing American Kidney Health” (AAKH) Executive Order, Eugene Lin and Paul Ginsburg co-authored a piece in the American Journal of Kidney Diseases analyzing the challenges and opportunities it will pose for large dialysis organizations. The executive order aims to disrupt status quo kidney care, shift the manner of treatment, increase home dialysis use, encourage more competition, and provide new payment models to care for the entire spectrum of kidney diseases.
Delivery System Reform
This year, the Centers for Medicare and Medicaid Services reported that the Medicare Shared Savings Program was successful in providing savings and demonstrated irrefutable effectiveness. The reports estimated $2.6 billion in gross savings in 2019 and $1.2 billion in net savings when accounting for shared-savings payments to participating Accountable Care Organizations (ACOs). In response to these reported savings, J. Michael McWilliams and Alice Chen crafted a two-part response published in Health Affairs, outlining the ways this assessment is misleading and overstates the true savings. In order to achieve true savings, they recommend a multitude of reforms including eliminating rebasing based on historical spending and increasing shared savings rates, among others.
Health Care Productivity
Dana Goldman, Neeraj Sood, John Romley, and Abe Dunn co-authored a piece assessing productivity growth in the treatment of a major chronic condition – type 2 diabetes. In this working paper, experts find that productivity of health care improved at an annualized rate of 2.2 percent from 2004-2012. This productivity improvement revealed itself mainly through a sizable decline in treatment costs, and partially in the form of better health outcomes. The study found costs decreased in the base analysis by 11.5 percent during this same time period, for an annualized rate of 1.3 percent.
Big Picture Healthcare Reform
With an eye to the future, Initiative experts continue to share their visions for the future of health policy. Fellows have encouraged plans to boost health insurance enrollment, provided insight into single-payer approaches, and been interviewed by various journals. In an interview, Matthew Fiedler offered the New England Journal of Medicine his perspective on the role the government should play in ensuring broad health insurance coverage, and how to encourage competition in health care provider markets.
The October issue of The American Journal of Managed Care featured an interview with Kavita Patel in honor of the their 25th anniversary. Patel discussed her ideas for a new Administration, lessons from the COVID-19 pandemic, and the future of capitated arrangements, or risk- or value-based arrangements like Medicare Advantage. Patel was interviewed again in late October citing positive changes in health care over the last two decades, underscored by the fact that more patients at every socioeconomic level have become increasingly aware of the high cost of care.
Eugene Lin co-authored a Health Affairs Blog discussing the toll of COVID-19 on hospitals especially those in low-income communities that are financially vulnerable. The authors warn of the impacts of hospital closures in these communities and propose a comprehensive plan to protect safety-net facilities from closure.
Paul Ginsburg provided analysis of Medicare for All and other single-payer approaches in an invited commentary published in the Journal of Ambulatory Care Management. Ginsburg outlined more immediate paths to cost reduction such as lowering administrative costs and provider prices. Lastly, Christen Linke Young co-authored a blog in Health Affairs that outlined ways to boost health insurance enrollment: alleviating the complexity and seeming unaffordability of health care, simplifying income rules, and creating auto-enrollment systems.
Looking at the future transition of the US healthcare system from a “fix-it-after-it breaks” to a “predicting, preventing, and detecting early disease” system, Dana Goldman penned a perspective in Scientific American on the promise of new multicancer blood tests that are in development. Goldman suggests these will be a “potent new weapon” that the US health system must be prepared to “marshall (these resources) in a new war on cancer.”

The Schaeffer Initiative held several convenings this year on critical policy areas, all held virtually in light of the COVID-19 pandemic. The transition to virtual events was sudden but proved to be more accessible for online participants and offered more flexibility in building panels. Seven events were held over the course of the year with over 6,255 live views. These events attracted speakers and audiences from around the world.
Wall Street Comes to Washington Healthcare Roundtable
March 31, 2020
Now in its 24th year, Paul Ginsburg’s signature roundtable event convenes Wall Street analysts from brokerage and investment management firms who cover health insurers and health care providers, especially hospitals, to discuss and analyze industry developments that are relevant to federal health policy. In bridging this discussion between Wall Street and Washington, this event provides policymakers a better understanding of how health care markets work and what changes are more impactful than others. This year’s event covered COVID-19, merger and acquisition trends, especially the push for vertical integration among insurers, pharmacy benefit managers, retail pharmacies, physician practices, and post-acute care providers; provider payment reform and the growing push for value-based payment; underlying health care spending and insurance premium trends; hospital consolidation and pricing; hospital-physician relations; the outlook for Medicare and Medicaid managed care; and other issues. Paul Ginsburg moderated.
Panelists: Matthew Borsch (Managing Director, BMO Capital Markets); Ricky Goldwasser (Managing Director, Morgan Stanley); George Hill (Managing Director, Deutsche Bank)
632 live views
1,110 total Views
A Short- and Long-Term Approach to COVID-19
April 17, 2020
The Schaeffer Initiative held an event focused on the short- and long-term approaches to COVID-19, featuring Dr. William A. Haseltine, known for his groundbreaking work on HIV-AIDS and pioneering application of genomics to drug discovery with Human Genome Sciences. Initiative Director Paul Ginsburg led a discussion focused on the spread of the virus, the populations who are most vulnerable, and what we can do now and, in the future, to limit the spread of COVID-19 to save lives.
752 live views
1,634 total Views
Health Insurance Auto-Enrollment
May 18, 2020
Before the COVID-19 pandemic, 30 million Americans were uninsured, but half of this population is eligible for insurance coverage through Medicaid or for financial assistance to buy coverage on the health insurance marketplace. Auto-enrollment is a method by which individuals are placed automatically into the health insurance coverage they are qualified for, and it has received support across the political spectrum. On May 18, the USC-Brookings Schaeffer Initiative for Health Policy, in partnership with the American Enterprise Institute, hosted a webinar discussing pathways to auto-enrollment that can help expand health insurance coverage. These strategies are likely to be even more necessary as the ranks of the uninsured increase as the economy contracts. The event was moderated by Paul Ginsburg.
Panelists: Christen Linke Young (Fellow, USC-Brookings Schaeffer Initiative for Health Policy); James Capretta (Visiting Fellow, American Enterprise Institute; Senior Fellow, Ethics and Public Policy Center); Stan Dorn (Director of the National Center for Coverage Innovation; Senior Fellow, Families USA); Lanhee J. Chen (David and Diane Steffy Fellow in American Public Policy Studies, Hoover Institution; Director of Domestic Policy Studies, Public Policy Program, Stanford University); David Kendall (Senior Fellow for Health Policy, Third Way)
1,267 live views
1,478 total Views
Innovation in Alzheimer’s Disease: Policies to Support Access to Treatments, Diagnostics, and Prevention
September 1, 2020
The past few decades have witnessed extraordinary biomedical breakthroughs in treatments for cardiovascular disease, cancer, and infectious diseases like HIV and hepatitis C. But progress against Alzheimer’s disease and related disorders remains frustratingly elusive. This is worrisome because without an effective intervention, dementia prevalence will triple over the next several decades, raising the specter of an aging America with healthy bodies housing deteriorating minds. On September 1, 2020, the Schaeffer Initiative hosted a webinar focusing on promising diagnostics and early treatments – even before cognitive symptoms are present – and the policy and payment challenges that must be addressed to evaluate these promising innovations and to support access. Leonard Schaeffer provided opening remarks followed by presentations by Paul Aisen and Darius Lakdawalla. Dana Goldman moderated both panels.
Clinical Panelists: Paul Aisen (Founding Director, USC Alzheimer’s Therapeutic Institute); Sharon Cohen (Medical Director, Toronto Memory Program and Division of Neurology, University of Toronto); Heather Snyder (Vice President, Medical and Scientific Relations, Alzheimer’s Association)
Policy Panelists: Darius Lakdawalla (Director of Research, USC Schaeffer Center); Steve Miller (Chief Clinical Officer, Cigna Corporation); Sarah Lenz Lock (Senior Vice President for Policy and Brain Health, AARP)
334 live views
1,848 total Views
3-Part Panel Series
On Healthcare Price Regulation
Honoring Uwe E. Reinhardt (1937-2017)
In partnership with the Center on Regulation and Markets at Brookings, the Initiative hosted a three-part panel series on health care price regulation honoring the late Uwe E. Reinhardt. In this series, experts from an array of backgrounds discussed the financial burden that health care places on households and how to pave a way forward. The late Uwe Reinhardt wrote and spoke extensively over many years in support of a larger role for the public sector in determining health care prices.
Part one focused on the question: Are US health care prices too high, too low, or some mix of the two? Part two discussed health care price regulation and public options and assessed different approaches to increasing the public role. Part three evaluated lessons from international experience in determining health care prices.
Are US Healthcare Prices too High, too Low, or Some Mix of the Two?
Part 1 – September 9, 2020
After Leonard Schaeffer’s introduction, Richard Besser, president of the Robert Wood Johnson Foundation and Tsung-Mei Cheng, Uwe’s wife and colleague, spoke. Tsung-Mei Cheng, who has written about initiatives in Germany and Taiwan to constrain health care prices, discussed Uwe’s thinking on these issues. The panel discussion that followed focused on the strengths and weaknesses of evidence used to assess health care prices, and what the evidence tells us regarding where prices are too high and how policymakers can respond. Louise Sheiner (The Robert S. Kerr Senior Fellow, Economic Studies, Policy Director, The Hutchins Center on Fiscal and Monetary Policy, the Brookings Institution) moderated.
Panelists: Melinda Buntin (Mike Curb Professor and Chair Department of Health Policy, Vanderbilt University Medical Center); Amitabh Chandra (Ethel Zimmerman Wiener Professor of Public Policy and Director of Health Policy Research, Harvard Kennedy School); Michael Chernew (Leonard D. Schaeffer Professor of Health Care Policy and Director of the Healthcare Markets and Regulation Lab, Department of Health Care Policy, Harvard Medical School); Daria Pelech (Principal Analyst, Health, Retirement, and Long-Term Analysis Division, Congressional Budget Office)
802 live views
1,229 total views
Healthcare Price Regulation and Public Options: Assessing Approaches to Increasing the Public Role
Part 2 – September 22, 2020
This panel discussion examined three commonly discussed approaches to expanding the government’s role in determining health care prices in private insurance markets: limits on out-of-network prices; comprehensive price regulation; and creating a public option. The panelists discussed how the effects of these different policy approaches might differ from each other and how they might compare to an approach that focused solely on improving competition in provider markets. Christen Linke Young moderated.
Panelists: Matthew Fiedler (Fellow, Economic Studies,
USC-Brookings Schaeffer Initiative for Health Policy); Benedic Ippolito (Research Fellow, The American Enterprise Institute); Cori Uccello (Actuary and Senior Health Fellow, The American Academy of Actuaries); Robert Murray (President, Global Health Payment, Former Executive Director, Maryland Health Services Cost Review Commission)
1,885 live views
2,085 total views
Lessons From International Experience in Determining Healthcare Prices
Part 3 – October 7, 2020
This panel examined the systems used to determine the prices of health care services in other developed countries. The panel provided a typology of the approaches commonly in use in other countries and examined a few specific systems in greater detail, with a particular focus on determining what lessons these other countries’ systems may have for policymakers in the United States. Paul Ginsburg served as moderator.
Panelists: Adam Elshaug (Visiting Fellow, Economic Studies, USC-Brookings Schaeffer Initiative for Health Policy); Miriam Laugesen (Associate Professor, Mailman School of Public Health, Columbia University); Chris Pope (Senior Fellow, Manhattan Institute); Reginald Williams II (Vice President, International Health Policy and Practice Innovations, The Commonwealth Fund)
503 live views
755 total Views
The Schaeffer Initiative for Health Policy successfully melds the data and analytic strengths of the USC Schaeffer Center with the policy and analytic expertise of Economics Studies at Brookings to provide insights on the nation’s most pressing health policy challenges. To ensure effective collaboration across the two organizations, Initiative experts conduct regularly scheduled calls and an annual strategic retreat at the Schaeffer Center in Los Angeles. These ongoing interactions allow the experts to set an annual plan and to seed new collaborative projects.
Leadership
Paul Ginsburg, PhD, Director of the USC-Brookings Schaeffer Initiative for Health Policy; Leonard D. Schaeffer Chair in Health Policy Studies, Brookings Institution; Director of Public Policy, USC Schaeffer Center; and Professor of Public Policy, USC Price School of Public Policy
Ginsburg is a well-known health policy expert, frequently called upon by government officials and agencies and the media. Since 2016, he has served as a Commissioner on the Medicare Payment Advisory Commission (MedPAC). From 1995 through 2013, Ginsburg founded and ran the Center for Studying Health System Change, and before that served as Executive Director of the predecessor to MedPAC, the Physician Payment Review Commission. He also served as Deputy Assistant Director at the Congressional Budget Office. In 2020, Ginsburg was named to the new National Academy of Medicine Committee on Emerging Science, Technology, and Innovation.
Dana P. Goldman, PhD, Leonard D. Schaeffer Director’s Chair, USC Schaeffer Center; Interim Dean, USC Price School of Public Policy; Distinguished Professor of Public Policy, Pharmacy, and Economics, USC School of Pharmacy and USC Price School of Public Policy; Nonresident Senior Fellow, Brookings
Goldman is the author of over 300 articles and book chapters, and has been published in leading medical, economic, health policy, and statistics journals. His research focuses on medical innovation and regulation, pharmacoeconomics, health care costs, public health, comparative effectiveness and outcomes, global health policy, and patient centered outcomes. An elected member of the National Academy of Medicine and the National Academy of Social Insurance and a research associate with the National Bureau of Economic Research, he has served as a policy advisor to the Congressional Budget Office, Covered California, the Fred Hutchinson Cancer Institute, and the NIH, and is a frequent expert on health issues in the media.
Loren Adler, MA, Associate Director, USC-Brookings Schaeffer Initiative for Health Policy
Adler’s research focuses on health insurance markets and provider pricing, and he is regularly called upon for technical assistance by federal and state lawmakers. Previously, Adler spent several years researching health care and fiscal policy at the Bipartisan Policy Center and Committee for a Responsible Federal Budget.
Fellows at Brookings
Matthew Fiedler, PhD, Fellow, USC-Brookings Schaeffer Initiative for Health Policy
Fiedler’s research focuses on the Affordable Care Act, Medicare, and provider payment. He previously served as Chief Economist for the Council of Economic Advisers in the Obama Administration, overseeing work on the creation and operation of the Health Insurance Marketplaces, health insurance regulation, Medicaid expansion, Medicare and private payment reform efforts, the Cadillac tax, and analyzed trends in health care costs and health insurance coverage.
Christen Linke Young, JD, Fellow, USC-Brookings Schaeffer Initiative for Health Policy
Young’s research focuses on the insurance reforms and Medicaid expansion under the ACA, and state and federal policies to promote health care coverage and affordability. She previously served as the Deputy Secretary for the North Carolina Department of Health and Human Services, overseeing the state’s Medicaid agency, improving coordination of social service benefits, and supporting child welfare outcomes. Before that, she was the Principal Deputy Director of the Center for Consumer Information and Insurance Oversight, implementing ACA market reforms and overseeing the operation of the federal Health Insurance Marketplace.
Fellows at Schaeffer Center
Alice Chen, PhD, Senior Fellow, USC Schaeffer Center; Associate Professor, USC Price School of Public Policy
Chen’s research focuses on improving the efficiency of health care markets. She examines how providers respond financial incentives, analyzes markets for pharmaceutical innovation, and considers how health spending jointly affects health and labor indicators. Her work has been published in top economics, policy, and medical journals, and it has been cited in major media outlets, including Business Week, CBS News, Forbes, The Atlantic, The New York Times, and The Washington Post.
Geoffrey Joyce, PhD, Director of Health Policy, Schaeffer Center; Chair of Pharmaceutical and Health Economics Department and Associate Professor, USC School of Pharmacy
Joyce’s research focuses on the impacts of Medicare Part D, prior authorization policies, and pricing in health care markets. His work has been widely published in peer-reviewed journals and featured in The Wall Street Journal, The Washington Post, Los Angeles Times, U.S. News & World Report, NBC Nightly News, CBS Evening News, National Public Radio, and other media.
Darius Lakdawalla, PhD, Director of Research, Schaeffer Center; Quintiles Chair in Pharmaceutical Development and Regulatory Innovation, USC School of Pharmacy; Professor, USC Price School
of Public Policy
Lakdawalla’s research focuses on the economics of risks to health, the value and determinants of medical innovation, the economics of health insurance markets, and the industrial organization of health care markets. He is a Research Associate at the National Bureau of Economic Research. Lakdawalla serves as Associate Editor for the Review of Economics and Statistics, The American Journal of Health Economics, and The Journal of Health Economics, and an editorial board member at the American Journal of Managed Care: Evidence-Based Diabetes and the American Journal of Managed Care: Evidence-Based Oncology.
Eugene Lin, MD, MS, Clinical and Resident Fellow, USC Schaeffer Center; Assistant Professor, Medicine and Health Policy & Management, Keck School of Medicine of USC and the USC Price School of Public Policy
Lin is a health services researcher with a focus on economic policies pertaining to nephrology. His research interests are in cost-effectiveness and assessing the impact of financial incentives on patient outcomes. He recently concluded a project studying the appropriateness of 30-day rehospitalizations in dialysis patients (NIH/NIDDK F32) and is studying the economic and social determinants of home dialysis drop-out (NIH/NIDDK K08). He also has interests in how Medicare policies affect the billing and delivery of health care by physicians and other providers, optimization of healthcare delivery, and has recently studied the cost-effectiveness of a multi-disciplinary care program in chronic kidney disease.
John Romley, PhD, Senior Fellow, Schaeffer Center; Associate Professor of Public Policy, USC Price School of Public Policy; Associate Professor of Pharmaceutical and Health Economics, USC School of Pharmacy
Romley’s research focuses on health care costs, public health, insurance markets and benefits design, and medical innovation and regulation. He participated in the first nationwide study of disparities in alcohol retailing in urban neighborhoods, with support from the Robert Wood Johnson Foundation, and was a co-investigator in an AHRQ-funded study that identified, categorized and evaluated efficiency measures in health care. He is the Managing Editor of Forum for Health Economics & Policy.
Neeraj Sood, PhD, Strategic Advisor to the Director, Schaeffer Center; Vice Dean for Research and Faculty Affairs and Professor of Public Policy, USC Price School of Public Policy
Widely published in peer-reviewed journals and frequently quoted in national media, Sood’s work focuses on pharmaceutical markets, health insurance, economics of innovation, Medicare, and global health. He has worked with the National Academies of Sciences, Engineering and Medicine on several projects, most recently in their report on the elimination of hepatitis B and C, and has provided insights to several government entities, including the Federal Trade Commission and the Senate.
Erin Trish, PhD, Associate Director, Schaeffer Center; Assistant Professor, USC School of Pharmacy; Nonresident Fellow, Brookings
Trish’s research focuses on the intersection of public policy and health care markets, with recent projects on surprise medical bills, prescription drug spending, health care market concentration, and health care reform. Her research has been funded by grants from the Robert Wood Johnson Foundation and Arnold Ventures, and published in leading health policy, health economics, and medical journals. She has testified in the California State Assembly and presented her research at numerous federal agencies, including the Congressional Budget Office, Federal Trade Commission, Office of the Assistant Secretary for Planning and Evaluation, and the Center for Consumer Information and Insurance Oversight.
Karen Van Nuys, PhD, Executive Director of the Value of Life Sciences Innovation project, USC Schaeffer Center; Research Assistant Professor, USC Price School of Public Policy
Van Nuys’s recent research focuses on the social value of novel therapies for heart failure and hepatitis C, the flow of funds in the pharmaceutical distribution chain, and the impact of commercial practices such as copay coupons and copay clawbacks on the utilization and cost of prescription drugs. Her work has been published in leading journals in economics, medicine, finance and health policy, and she is frequently called upon by the media for expert comment.
Contributing Scholars
Mark Hall, JD, Nonresident Senior Fellow, Brookings; Fred D. & Elizabeth L. Turnage Professor of Law, Wake Forest University
Hall is one of the nation’s leading scholars in the areas of health care law, public policy, and bioethics. He has been published in law reviews at Berkeley, University of Chicago, Duke, University of Michigan, University of Pennsylvania, and Stanford, and teaches at the Wake Forest Graduate Program for Bioethics and its MBA program.
Jason Levitis, JD, Nonresident Fellow, Brookings
From 2009-2017, Levitis served in various senior positions at the U.S. Treasury Department, leading ACA implementation and the state innovation waiver process.
Steven Lieberman, MPhil, MA, Nonresident Fellow, Brookings
Lieberman has had a decades-long career in Washington with senior positions at the Office of Management and Budget, the Congressional Budget Office, and the Centers for Medicare & Medicaid Services. In between government service, Lieberman worked in executive roles at large HMO plans. He is currently President of Lieberman Consulting and a Senior Advisor to the Bipartisan Policy Center.
Kavita Patel, MD, MPH, Nonresident Fellow, Brookings; Practicing Primary Care Physician, Sibley Memorial Hospital
Patel, a practicing primary care physician, also serves as an Advisor to the Bipartisan Policy Center and a member of the Health and Human Services Physician-Focused Payment Model Technical Advisory Committee. Previously she worked in the Obama Administration as director of policy for the Office of Intergovernmental Affairs and Public Engagement at the White House. Prior to that Patel was Deputy Director on Health for Senator Edward Kennedy.
Bruce Steinwald, MBA
Steinwald is a health economist with decades of experience in academia, government, and private consulting. He currently operates a small consulting practice in Washington and serves on the Physician-Focused Payment Model Technical Advisory Committee, which advises the Secretary of Health and Human Services on Medicare payment reforms.

Media Highlights

Experts from the Schaeffer Initiative are regularly in touch with media for comment on trending health care issue, especially during the COVID-19 pandemic. With expertise on Medicare, Medicaid, the Affordable Care Act, and pharmaceutical pricing, among other issues, media outlets rely on Initiative expertise for timely, independent research, analysis, and background discussion on salient topics under consideration in Washington and across the nation. Additionally, media members frequently attend Schaeffer Initiative conferences/webinars.
February 2020
Research by Loren Adler cited on NPR: Doctors push back as Congress takes aim at surprise medical bills (February)
Christen Linke Young in Kaiser Health News: Feds slow down, but don’t stop Georgia’s contentious effort to ditch ACA marketplace
Paul Ginsburg on NPR: A top restaurateur thinks single payer health care could boost his bottom line
March 2020
Christen Linke Young in Kaiser Health News: Pence leaves out key details about health coverage of coronavirus testing
April 2020
Loren Adler in Consumer Reports: Paying for healthcare in the age of coronavirus. In an article laying out strategies to help pay for care
“Treatments for COVID-19 could be especially expensive if you need to go to the ER or are admitted to the hospital.” – Loren Adler, Consumer Reports
Dana Goldman on NPR: What would it take to bring more pharmaceutical manufacturing back to the U.S.?
Neeraj Sood in The Wall Street Journal: More L.A. County residents likely infected with coronavirus than thought, study finds
“The good news is that the fatality rate is lower than what we thought it would be. But the fatality rate is not the only number we should focus on. We are very early in the epidemic, and many more people in L.A. could be infected.” – Neeraj Sood, The Wall Street Journal
Dana Goldman in Fox News Online: Return to work? States, counties play it safe amid coronavirus uncertainty
“These decisions about opening up the economy need to be made and it doesn’t make sense to make it at a national level. It should be made at a local level, and the governors should probably rightly devolve it to some of the localities.” – Dana Goldman, Fox News Online
Loren Adler in Politico: ‘Surprise’ billing fix could hitch ride on next coronavirus relief bill
June 2020
Christen Linke Young in Business Insider: Trump and Congress tried to make coronavirus testing and treatment free, but people are still getting big bills when they go to the hospital
Darius Lakdawalla in Associated Press: Pooled testing for COVID-19 holds promise, pitfalls
Darius Lakdawalla in Forbes: Pooled COVID-19 testing may help us get back to work and school
Christen Linke Young in Time: Did you lose your health insurance amid the coronavirus pandemic? You may have other options
July 2020
Loren Adler in Politico: White House bids for surprise billing fix ahead of next rescue package
Paul Ginsburg in The Washington Post: When doctors opt out of Medicare, the change can be tough for patients
“If you’re a large primary care practice, private insurers are really going to want to have you in their network, and they’re willing to pay more than they might pay an individual solo practitioner who they’re not as concerned [with] because it’s only one physician.” – Paul Ginsburg, The Washington Post
Christen Linke Young in Vox: How Trump gave insurance companies free rein to sell bad health plans
Geoffrey Joyce in The Los Angeles Times: Trump taps Kodak to bring stability to the drug market
Part one focused on the question: Are US health care prices too high, too low, or some mix of the two? Part two discussed health care price regulation and public options and assessed different approaches to increasing the public role. Part three evaluated lessons from international experience in determining health care prices.
August 2020
Christen Linnke Young in the Atlanta Journal-Constitution: Kemp proposal drops big changes to Georgia Obamacare
Jason Levitis on NPR: Rule change gives laid-off workers more time to sign up for COBRA insurance.
Matthew Fiedler in The Incidental Economist: What can be done
about upcoding?
Karen Van Nuys in PolitiFact: Trump inflates insulin help for seniors
September 2020
Christen Linke Young in The New York Times: Surprise bills for COVID-19 tests
“This is legitimately a confusing area, and the coding is all evolving. Even if you’re an insurer or provider operating in good faith, and think you know what the rules are, figuring out how to identify relevant claims is a hurdle.” – Christen Linke Young on surprise bills for COVID tests, The New York Times
Kavita Patel in Politico: Biden wants to restore Obamacare. He may have trouble
Christen Linke Young in the Atlanta Journal-Constitution: Kemp’s plan to block the federal ACA insurance exchange under fire
Paul Ginsburg in The Health Care Blog: Hospitals must give up power to save healthcare
Erin Trish in Fact Check: Viral post wrongly ties cost drop to Trump’s ‘Prescription Bill’
October 2020
Dana Goldman in Los Angeles Times: Trump says he has a better plan for preexisting conditions. He doesn’t
Kavita Patel in The American Journal of Managed Care spotlight: Could COVID-19 become a policy tipping point
Erin Duffy and Loren Adler in The American Journal of Managed Care: Surprise medical bills drive up health premiums for all
Christen Linke Young in Yahoo Finance: Americans are more concerned about access to health care
Loren Adler in Salon: On health care, Trump’s claims don’t add up.
John Romley in The Los Angeles Times: Many Californians, particularly Blacks residents, would skip taking the COVID vaccine today, study finds
Erin Trish in California Healthline: Dialysis industry on the defense against Prop 23
November 2020
Christen Linke Young in The Los Angeles Times: The Supreme Court Obamacare case centers on technicalities, but much more is at stake
Paul Ginsburg on NPR: Hit with an unexpectedly high medical bill, here’s how a savvy patient fought back
Loren Adler in US News & World Report: Insured patients are getting surprise bills after colonoscopies
Erin Trish in Kaiser Health News: Medicare open enrollment is complicated. Here’s how to get good advice
December 2020
Loren Adler in The New York Times: Why ambulances are exempt from the surprise-billing ban
Eugene Lin in Scientific American: Should your kidney doctor have a financial stake in dialysis

Schaeffer Initiative White Papers
Capping prices or creating a public option: How would they change what we pay for health care? (November 19, 2020) USC-Brookings Schaeffer Initiative for Health Policy, Matthew Fiedler
Federal policy options to realize the potential of APCDs (October 23, 2020) – USC-Brookings Schaeffer Initiative for Health Policy, Matthew Fiedler and Christen Linke Young
Taking a broader view of “junk insurance” (July 6, 2020) – USC-Brookings Schaeffer Initiative for Health Policy, Christen Linke Young
Making ACA enrollment more automatic for the newly unemployed (May 28, 2020) – USC-Brookings Schaeffer Initiative for Health Policy, Christen Linke Young and Sobin Lee
Productivity growth in treating a major chronic health condition (May 14, 2020) – USC-Brookings Schaeffer Initiative for Health Policy and Hutchins Center on Fiscal and Monetary Policy’s Productivity Measurement Initiative, John A. Romley, Dana Goldman, Neeraj Sood, and Abe Dunn
How well could tax-based auto-enrollment work? (April 14, 2020) –
USC-Brookings Schaeffer Initiative for Health Policy, Christen Linke Young and Sobin Lee
Georgia’s 1332 waiver violates the ACA and cannot lawfully be approved (January 23, 2020) – USC-Brookings Schaeffer Initiative for Health Policy, Christen Linke Young, Jason Levitis
Select Journal Articles
Competing visions for the future of health policy (September 24, 2020) – New England Journal of Medicine, Matthew Fiedler
Policies to address surprise billing can affect health insurance premiums (September 11, 2020) – American Journal of Managed Care, Erin L. Duffy, Bich Ly, Loren Adler, Erin Trish
Payer mix among patients receiving dialysis (September 1, 2020) – JAMA, E. Lin, K.F. Erickson
Commentary on “Health spending under single-payer approaches” (July/September 2020) – Journal of Ambulatory Care Management, Paul Ginsburg
Consolidation by any other name? The emergence of clinically integrated networks (August 20, 2020) – Health Services Research, M.S. Ridgely, J. Timbie, E. Duffy, L. Wolf, C. Buttorff
The “Advancing American Kidney Health” Executive Order: Challenges and opportunities for the large dialysis organizations (August 4, 2020) – American Journal of Kidney Diseases, Eugene Lin, Paul B. Ginsburg, Glenn M. Chertow, Jeffrey S. Berns
Early delays in insurance coverage and long-term use of home-based peritoneal dialysis (July, 2020) – Medical Care, E. Lin, G.M. Chertow, J. Bhattacharya, D. Lakdawalla
Out-of-network air ambulance bills: Prevalence, magnitude, and policy solutions (June 11, 2020) – The Milbank Quarterly, Erin C. Fuse Brown, Erin Trish, Bich Ly, Mark A. Hall, Loren Adler
Getting Americans back to work (and school) with pooled testing (May 5, 2020) – USC Schaeffer Center White Paper, D. Lakdawalla, E. Keeler, D. Goldman, E. Trish
Prevalence and characteristics of surprise out-of-network bills from professionals in ambulatory surgery centers (April 15, 2020) – Health Affairs, Erin Duffy, Loren Adler, Paul Ginsburg, Erin Trish
The price and spending impacts of limits on payments to hospitals for out-of-network care (March 12, 2020) Rand Research Report, E.L. Duffy, C. Whaley, C. White
The ACA’s individual mandate in retrospect: What did it do, and where do we go from here? (March 2, 2020) – Health Affairs, Matthew Fiedler
Health care in President Trump’s fiscal year 2021 budget (February 13, 2020) – JAMA Insight, Matthew Fiedler, Loren Adler, Christen Linke Young
Policy issues in dialysis care (January-February 2020) – Seminars in Dialysis, E. Lin, K. Erickson, W. Windelmayer
Does Medicare coverage improve cancer detection and mortality outcomes? (January 12, 2020) – Journal of Policy Analysis and Management, Rebecca Myerson, Reginald Tucker-Seeley, Dana Goldman, Darius Lakdawalla
Conflicts of interest in dialysis: A barrier to policy reforms (January 3, 2020) – Seminars in Dialysis, A. Glickman, Eugene Lin, J.S. Berns
Four years into MACRA: What has changed? (January 2020) – Seminars in Dialysis, J. Cheng, J. Kim, S.D. Bieber, Eugene Lin
Select Blogs / Commentaries / Podcasts
Balancing lower U.S. prescription drug prices and innovation – Part 2 (November 25, 2020) – Health Affairs blog, Steven M. Lieberman, Paul B. Ginsburg, and Kavita Patel
Balancing lower U.S. prescription drug prices and innovation – Part 1 (November 24, 2020) – Health Affairs blog, Steven M. Lieberman, Paul B. Ginsburg, and Kavita Patel
Understanding the latest ACO “savings”: Curb your enthusiasm and sharpen your pencils – Part 2 (November 13, 2020) – Health Affairs blog, J. Michael McWilliams and Alice Chen
Understanding the latest ACO “savings”: Curb your enthusiasm and sharpen your pencils – Part 1 (November 12, 2020) – Health Affairs blog, J. Michael McWilliams and Alice Chen
The COVID-19 vaccines are coming. Here’s how they should be rolled out. (October 25, 2020) – Los Angeles Times, Bob Kocher and Dana Goldman
What can be done to improve all-payer claims databases? (October 23, 2020) – USC-Brookings Schaeffer Initiative for Health Policy blog, Matthew Fiedler and Christen Linke Young
Silver-Loading Likely To Continue Following Federal Circuit Decision On CSRs (October 13, 2020) – Health Affairs blog, Aviva Aron-Dine and Christen Linke Young
A Supreme Court decision to strike down the ACA would create chaos in the health care system (October 13, 2020) – USC-Brookings Schaeffer Initiative for Health Policy blog, Christen Linke Young
High air ambulance charges concentrated in private equity-owned carriers (October 13, 2020) – USC-Brookings Schaeffer Initiative for Health Policy blog, Loren Adler, Kathleen Hannick, and Sobin Lee
Free COVID-19 vaccines: Not enough to guarantee acceptance, especially among Black Americans (October 8, 2020) – The Evidence Base, Dana Goldman, Matthew Crane, and John Romley
Surprise medical bills increase costs for everyone, not just for the people who get them (October 2, 2020) – The Conversation, Erin Duffy, Erin Trish, Loren Adler
GAO report sheds additional light on misleading and deceptive
marketing practices among non-compliant health plans (September 25, 2020) – USC-Brookings Schaeffer Initiative for Health Policy blog, Kathleen Hannick and Christen Linke Young
Sharing drug rebates with Medicare Part D patients: Why and how (September 14, 2020) – Health Affairs blog, Steven M. Lieberman, Paul B. Ginsburg, and Erin Trish
The COVID-19 Vaccine Model Needs to Prioritize ‘Superspreaders.’ Here is Why (September 3, 2020) – The Conversation, Dana Goldman, D. Conti, M. Kahn
How To Boost Health Insurance Enrollment: Three Practical Steps That Merit Bipartisan Support (August 17, 2020) – Health Affairs Blog, Christen Linke Young, James C. Capretta, Stan Dorn, David Kendall, Joseph R. Antos
Fixed indemnity health coverage is a problematic form of “junk insurance” (August 4, 2020) – USC-Brookings Schaeffer Initiative for Health Policy blog, Christen Linke Young and Kathleen Hannick
The laws governing COVID-19 test payment and how to improve them (July 13, 2020) – USC-Brookings Schaeffer on Health Policy blog, Loren Adler and Christen Linke Young
COVID-19 Myths (July 8, 2020) – The Conversation, Geoffrey Joyce
Group testing for coronavirus – called pooled testing – could be the fastest and cheapest way to increase screening nationwide (July 2, 2020) – The Conversation, Darius Lakdawalla and Erin Trish
Preparing for the next COVID-19 crisis: A strategy to save safety-net hospitals (June 22, 2020) – Health Affairs blog, Eugene Lin, Peter Reese, and Meera N. Harhay
Adapting Medicare Advantage bidding for COVID-19 related uncertainty on claims: A proposal (May 18, 2020) – USC-Brookings Schaeffer on Health Policy blog, Steven M. Lieberman
To get Congress and the economy back to work, jump in the testing pool (May 13, 2020) – The Hill, Darius Lakdawalla and Dana Goldman
Early detection: A new front in the war on cancer (May 6, 2020) – Scientific American, Dana Goldman
Where is big data when we need it most? (April 23, 2020) – The Hill, C. Worsham, A. Jena, Dana Goldman
How California’s smog alert system could be adapted to fight the coronavirus (April 19, 2020) – Los Angeles Times, Dana Goldman and Aaron Edlin
Responding to COVID-19: Using the CARES Act’s hospital fund to help the uninsured, achieve other goals (April 11, 2020) – Health Affairs blog, Christen Linke Young, Stan Dorn, Loren Adler, Cheryl Fish-Parchman, Tara Straw
Hospitals closed to prepare for COVID-19. It is time to reopen most of them (April 10, 2020) – The Evidence Base, Dana Goldman, Darius Lakdawalla, and Erin Trish
How the CARES Act affects COVID-19 test pricing (April 9, 2020) – USC-Brookings Schaeffer Initiative for Health Policy blog, Loren Adler
The Elijah E. Cummings Lower Drug Costs Now Act: How it would work, how it would affect prices, and what the challenges are (April 9, 2020) – The Commonwealth Fund, Paul Ginsburg, Steven Lieberman
States will need more fiscal relief. Policymakers should make that
happen automatically (April 2, 2020) – USC-Brookings Schaeffer Initiative for Health Policy blog, Matthew Fiedler and Wilson Powell III
Misleading marketing of short-term health plans amid COVID-19 (March 24, 2020) – USC-Brookings Schaeffer Initiative for Health Policy blog, Christen Linke Young and Kathleen Hannick
COVID-19’s painful lesson in leadership (March 23, 2020) – Global Health Now, Steven M. Lieberman
What do I do if I lose my job-based health insurance? (March 17, 2020) – USC-Brookings Schaeffer Initiative for Health Policy blog, Christen Linke Young
It’s dangerous to test only the sick (March 15, 2020) – The Wall Street Journal, Neeraj Sood
What are the health coverage provisions in the House coronavirus bill? (March 13, 2020) – USC-Brookings Schaeffer Initiative for Health Policy blog, Matthew Fiedler, Christen Linke Young, Loren Adler
The Affordable Care Act at 10 years, podcast (March 13, 2020) – The Brookings Cafeteria, Christen Linke Young
Health care priorities for a COVID-19 stimulus bill: Recommendations to the administration, Congress, and other federal, state, and local leaders from public health, medical, policy and legal experts (March 12, 2020) – Health Affairs blog, Howard P. Forman, Elizabeth Fowler, Megan L. Ranney, Ruth J. Katz, Sara Rosenbaum, Kavita Patel, Abbe R. Gluck, Christen Linke Young, Brendan G. Carr, Erica Turret, Suhas Gondi, Timothy Jost, Adam L. Beckman
Comments submitted on HHS Notice of Benefit and Payment Parameters for 2021 (March 2, 2020) – USC-Brookings Schaeffer Initiative for Health Policy Op-Ed, Christen Linke Young and Jason Levitis
There are clear, race-based inequalities in health insurance and health outcomes (February 19, 2020) – USC-Brookings Schaeffer Initiative for Health Policy blog, Christen Linke Young
Obesity, second to smoking as the most preventable cause of US deaths, needs new approaches (January 27, 2020) – The Conversation, Dana Goldman
Remanding Texas v. U.S. to the lower court prolongs harms to consumers and the health care industry (January 3, 2020) – USC-Brookings Schaeffer Initiative for Health Policy blog, Christen Linke Young
You must be logged in to post a comment.