Gestational diabetes mellitus (GDM) is the most common complication of pregnancy in the world, affecting more than 1 in 10 pregnancies worldwide in 2019. GDM has implications for both maternal/child health as well as rising rates of chronic disease, as it not only significantly elevates risks during childbirth (due, for instance, to the higher incidence of macrosomia – large babies) but is also associated with later development of type 2 diabetes in the mother. As a result, understanding how to manage GDM – as well as support lifestyle changes that may help prevent future diabetes diagnoses – is a critical concern for women’s health. One potential approach may be to integrate mobile health (mHealth) into the care model for GDM, leveraging successful mHealth platforms to support patient care and behavioral change in related areas of weight control, chronic disease management, and remote health care delivery.
Singapore is an ideal setting for piloting these approaches, given the relatively high population prevalence (nearly 19% of pregnant women experiencing the condition), and almost universal rates of internet access. In a recent study with our colleagues Jananie Audimulam and Emily Sullivan (both from National University of Singapore), and Claudia Chi and Yew Tong Wei (both from National University Hospital, Singapore), we explored the appropriateness and acceptability of mHealth interventions for GDM care among pregnant women with GDM as well as their health care providers from two specialized GDM clinics at one of the largest public maternity units in Singapore. The study combined both quantitative and qualitative data collection on their current and preferred GDM care, information, and support. Two hundred and sixteen women with GDM participated in the cross-sectional survey, and semi-structured interviews were conducted with fifteen women. We also interviewed a range of health care providers treating patients with GDM who were from different specialties, including obstetrics and gynecology, diabetes care nursing, and dietetics.
Our results showed that women, especially those who are working, experienced diverse individual and structural barriers in managing GDM, including a lack of reminders for blood glucose monitoring and diet control, as well as having insufficient time for exercise. Most were already receiving support and information from the GDM clinic or web-based sources (Figure 1).
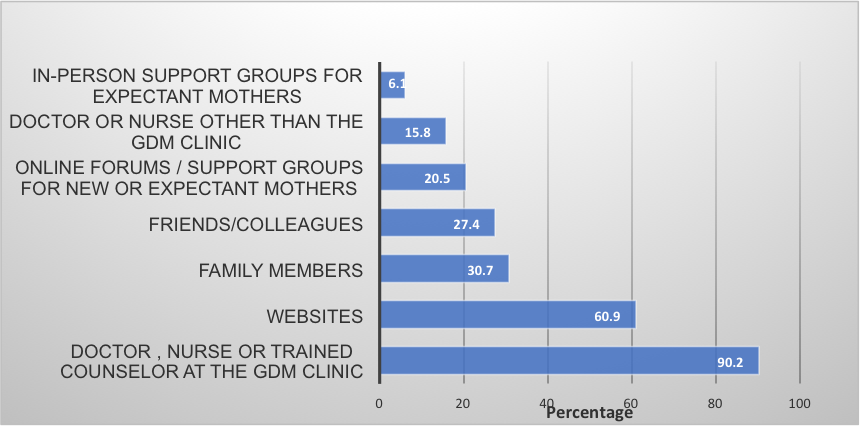

In surveys as well as interviews, most women expressed a strong preference for receiving information directly from health care providers rather than popular websites or informal sources. The qualitative interview data further revealed, however, that while most women preferred having a provider be their primary source of information and support, they would prefer to receive such interventions via a smartphone app rather than in person. Women raised the need for broader support features than usually possible during (limited) face-to-face consultations, including more extensive information on GDM, diet, and exercise (ideally curated by care providers); regular blood glucose test reminders; a platform to record and interpret trends in blood glucose readings; and a means to communicate more easily with care providers (Figure 1). Participants felt such a smartphone app would be a feasible solution for GDM management during pregnancy, and as importantly, might also help them to maintain lifestyle changes post-partum.
Health care providers across disciplines also agreed that a smartphone app would be a convenient and supportive platform for patients with GDM control. From the provider perspective, they highlighted the clinical value of directly linking the patient and provider interface, particularly with respect to information about blood glucose test results in terms of increasing the accuracy and timeliness of monitoring (relative to methods such as paper-based tracking). From the patient perspective, they stressed the importance of being a user-friendly and affordable means of intervention.
Based on this study’s findings, our collaborators have developed a smartphone app linked to a phone-based glucometer and adapted to lifestyle change recommendations that are sensitive to the local context. This is already being piloted in Singapore in a trial that will reveal vital information about the effectiveness and cost-effectiveness of such an intervention. In the current pandemic situation, as health system resources are further constrained, the value of such an app may be heightened further, especially for patients for whom telehealth may be the most viable option.

You must be logged in to post a comment.