While a safe and effective COVID-19 vaccine is widely seen as key to ending the pandemic, polling over the last several months has shown that many Americans would not get a vaccine if one were available. In the U.S. and other countries, vaccine “hesitancy” is a growing public health challenge. In addition, in the COVID-19 context, some have cited safety concerns as a source of hesitancy.
The current economic downturn may also be a significant barrier to the use of a COVID-19 vaccine, though, especially among lower-income individuals. Research in other contexts has shown the role of cost as a demotivator for vaccination. In addition, news reports of high costs for supposedly free COVID-19 tests may be playing a role in shaping perceptions about pandemic-associated healthcare costs. With this potential for cost to be a factor, officials at Operation Warp Speed recently announced their intention to make a COVID-19 vaccine free for all Americans.
Perceptions of high costs could be contributing to the overall hesitancy found in opinion polls. We explored this issue through the UAS Understanding Coronavirus in America Study, asking participants how much they would be willing to pay for a COVID-19 vaccine. A person who reports a “willingness to pay” of $20, for example, would use a vaccine if the cost were $19 or even $20, but not if the cost were $21. A person with a high willingness to pay perceives greater benefits from a vaccine.
Cost does matter. For example, we estimate that half of adults in the U.S. would use a vaccine if the cost were $50, but only a quarter would if the cost were $75. Willingness to pay for a vaccine is higher among those with higher education levels, those of older age, and those identifying as Democrats.
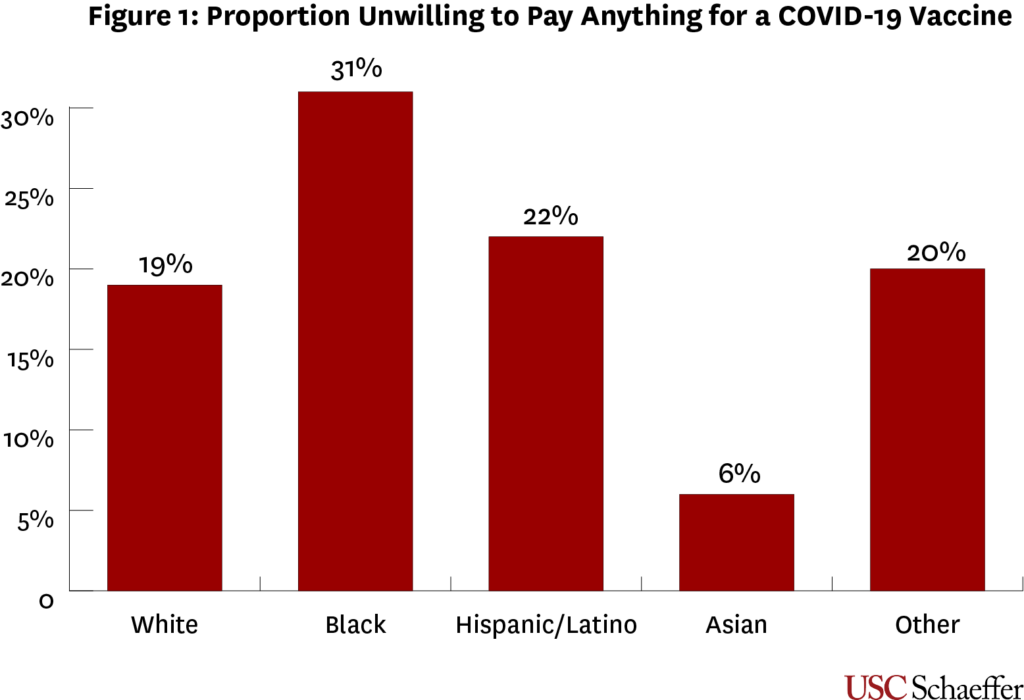
Yet, cost is not the whole story. One out of five adults reportedly would not pay anything for a COVID-19 vaccine. We posit these individuals would be unlikely to use a vaccine, and cost is not the reason. Something else is driving their hesitancy.
There is a strong pattern to this perspective in terms of race and ethnicity. As Figure 1 shows, 31% of Black Americans would be unwilling to pay anything for a vaccine, compared to 19% of whites, 22% of Hispanics, and 6% of Asians.
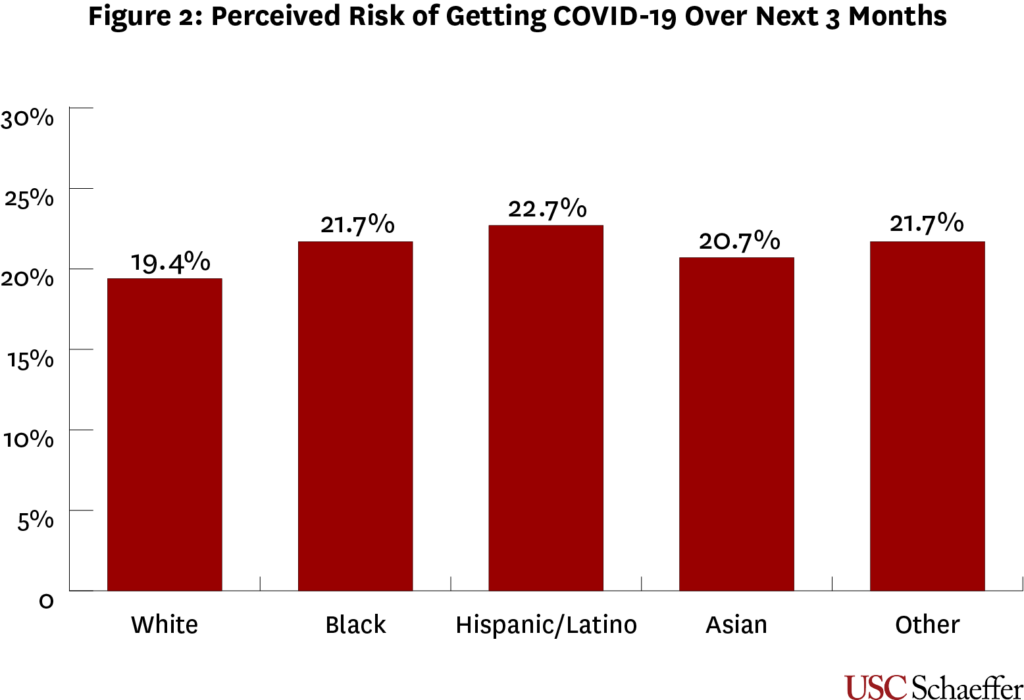
One possible explanation for this pattern is that Blacks perceive a lower risk from COVID-19 than other groups do. In reality, people of color have borne a disproportionate share of the burden of this disease in the U.S. and Black Americans recognize this reality. As shown in Figure 2 based on our UAS survey, Black Americans believed there was a 21.7% chance of getting COVID-19 over the next three months, a slightly higher risk than was perceived by whites (19.4%).
Taken together, these results indicate that the incentive offered by a free COVID-19 vaccine may be powerful in encouraging adoption, but it is not sufficient to eliminate racial inequity in vaccine use.
Our findings may be contextualized by a long history of mistreatment of Black Americans throughout the institution of American medicine, exemplified by but not limited to the profoundly unethical Tuskegee Study. Due to such publicized examples of mistreatment, as well as negative individual and community interactions with healthcare systems, prevalent feelings of distrust towards medical institutions have been well-documented among Black Americans.
Such attitudes unfortunately can perpetuate racial inequities in medicine and health through various avenues. Due to distrust, Black Americans are less likely to participate in clinical trials, less likely to be organ donors, and less likely to adopt influenza vaccination practices.
While inequities are unjustifiable under any conditions, the pandemic’s disproportionate impact on communities of color further highlights the importance of prioritizing trust-building and transparency in the process of vaccine development and deployment.
These findings are relevant in light of ongoing national conversations on pricing of a COVID-19 vaccine. In recent weeks, officials from Operation Warp Speed have announced their intention that a COVID-19 vaccine should be free for all Americans. Despite this, reports have shown a lacking tandem effort to combat vaccine hesitancy and ensure widespread adoption of the eventual product.
While concerns over widespread adoption of a vaccine must address questions of safety and efficacy, we have found that cost is a significant dimension as well. Beyond this, though, we find that cost does not fully account for hesitancy towards a COVID-19 vaccine, especially among Blacks.
More attention should be paid by federal, state, and local health agencies towards effectively stemming concerns of safety and transparency in vaccine approval, handling, and delivery. Improving our national messaging surrounding development and deployment is especially critical in the context of communities of color, especially Black Americans, who may be distrustful of medical institutions due to historical wrongs. Such steps are essential to fostering trust towards improving racial equity in our pandemic response.
Acknowledgment
The project described in this paper relies on data from survey(s) administered by the Understanding America Study, which is maintained by the Center for Economic and Social Research (CESR) at the University of Southern California. The content of this paper is solely the responsibility of the authors and does not necessarily represent the official views of USC or UAS. The collection of the UAS COVID-19 tracking data is supported in part by the Bill & Melinda Gates Foundation and by grant U01AG054580 from the National Institute on Aging, and many others.
You must be logged in to post a comment.