Difference between Traditional Medicare and Medicare Advantage in Dementia Care
Symptoms of dementia most often appear at older ages and disease progression leads to substantial healthcare needs and expenses. Dementia medical care needs are primarily addressed by Medicare, the main insurer for the roughly 57 million people ages 65 and older in the United States in 2023. Medicare beneficiaries are enrolled in either traditional Medicare (TM) or the private plan alternative, Medicare Advantage (MA), and MA plans have grown in popularity, increasing from 13% of all Medicare beneficiaries in 2005 to nearly 50% in 2023 (Jacobson et al., 2023). Yet despite this significant growth in enrollment in private Medicare plans, much is not yet understood about how dementia care differs for beneficiaries enrolled in the private plans.
Researchers can now examine these questions using Medicare Encounter data that has recently become available for study. Researchers at the USC Schaeffer Center for Health Policy & Economics have taken the lead in comparing prevalence and incidence rates in dementia diagnoses, and healthcare utilization and subsequent mortality among persons living with dementia who are enrolled in either MA or TM.
How is Medicare Advantage different than traditional Medicare?
In TM, healthcare providers receive a fee for each healthcare service a beneficiary receives. In MA, the federal government instead pays MA plans a fixed (also known as capitated) monthly amount per beneficiary to cover the expected costs of the healthcare services of the patient population. For MA plans, the size of capitated payments is determined through risk adjustment: the federal government sets payments to reflect the health status of a plan’s members. Risk adjustment helps ensure that plans do not have financial incentives to avoid sicker populations. By increasing payment for people with certain conditions, these adjustments may also create incentives for MA plans to make and document enrollee diagnoses, which could ultimately lead to differential diagnosis of otherwise similar persons in MA and TM.
Is diagnosis of dementia different in Medicare Advantage and traditional Medicare?
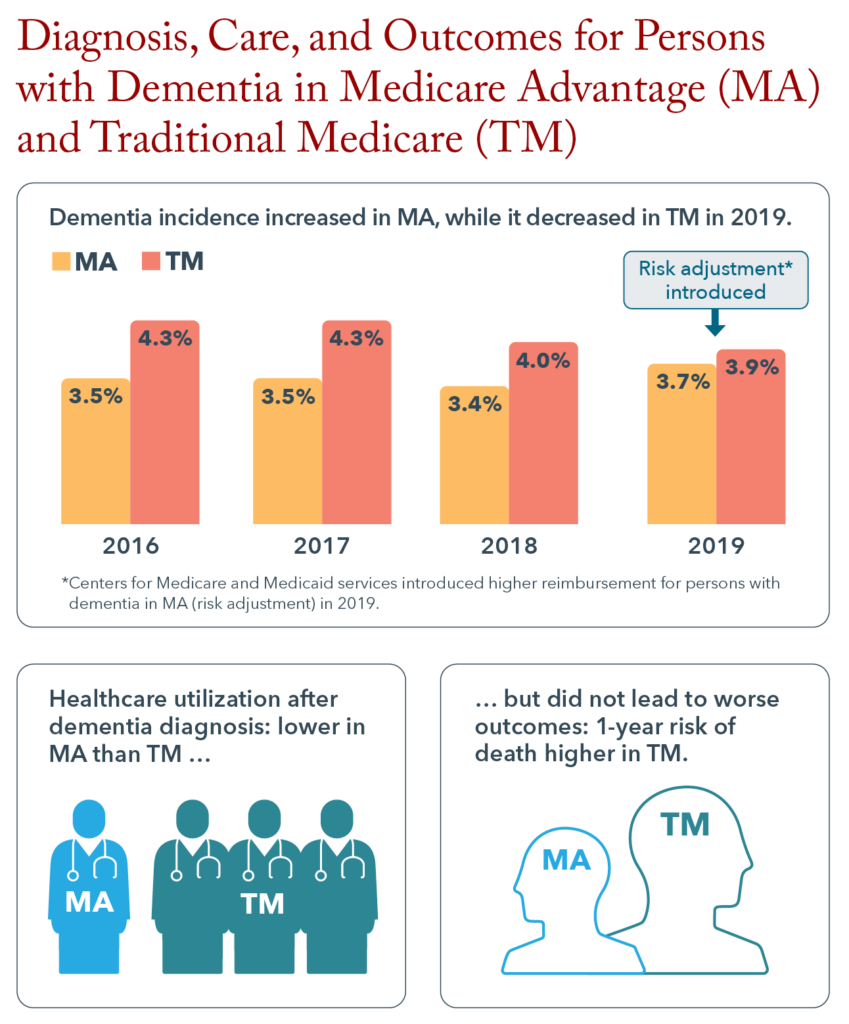
To examine whether MA benefit and payment structures may impact rates of dementia diagnosis, Schaeffer Center researchers compared diagnoses in MA and TM before and after the inclusion of dementia in MA risk adjustment. Medicare reintroduced risk adjustment for Alzheimer’s disease and related dementias (ADRD) in 2019, and ADRD was used to adjust 2020 MA plan payments. Haye et al. (2023) compared dementia diagnoses in MA and TM in 2017, before the introduction of ADRD-based risk adjustment. Using an MA sample that was designed to match the health and demographic characteristics of the TM population, the study found that in 2017, beneficiaries in MA were less likely than beneficiaries in TM to have a dementia diagnosis. Zissimopoulos et al. (2023) examined dementia diagnoses before, at, and after the introduction of ADRD-based risk adjustment. They found that among MA beneficiaries, 3.5% of enrollees received a new diagnosis of dementia in 2016 and that rates remained steady through 2018 before increasing to 3.7% in 2019 – the first year that dementia was added to risk adjustment calculations. This diagnostic increase in MA contrasted with a steady decrease in new dementia diagnoses among TM beneficiaries, from 4.3% in 2016 to 3.9% in 2019. These divergent trends raise the possibility of improved detection within MA plans as a result of the financial incentive to detect and diagnose dementia. However, more research is needed to determine whether the change reflects improved detection or has led to potentially inappropriate overdiagnosis of dementia.
Is healthcare use by persons living with dementia different in Medicare Advantage and traditional Medicare?
Other studies have documented different rates of healthcare use in MA and TM but few have examined medical care for persons with complex healthcare needs, such as persons living with dementia. Jacobson et al. (2023) investigated healthcare utilization among comparable MA and TM beneficiaries, both before and after a dementia diagnosis. They found hospitalization rates and outpatient visits were comparable in MA and TM from 12 months to 4 months before diagnosis. In the 3 months leading up to a dementia diagnosis, both outpatient doctor visits and inpatient hospital stays were higher for beneficiaries enrolled in TM compared to MA. At the month of diagnosis, TM beneficiaries had higher rates of hospitalizations compared to MA beneficiaries; 36.5% of TM enrollees were hospitalized compared to 25% of MA beneficiaries. Additionally, TM beneficiaries had 1.6 more outpatient visits than their MA counterparts during the month of diagnosis. This higher healthcare use by TM enrollees continued for months after a dementia diagnosis, as well.
What is the rate of mortality after a dementia diagnosis?
A critical question is whether the differences in the use of health care of MA and in TM beneficiaries around the time of a dementia diagnosis ultimately led to different health outcomes, including mortality. Jacobson et al. (2023) analyzed one-year mortality rates after a dementia diagnosis. They found there was a 16% increase in the odds of dying within one year of a dementia diagnosis for TM beneficiaries, compared MA beneficiaries. The factors contributing to different mortality rates remain unknown. One possibility is better dementia care management for MA beneficiaries compared to TM, although direct evidence for this hypothesis is needed.
What research do we need going forward?
Well-managed care is vital for helping people with dementia maintain quality of life and for potentially reducing adverse outcomes. USC Schaeffer Center researchers found Medicare payment structures impact dementia diagnosis and the healthcare received, while additional research is needed to explore how and for whom in order to identify opportunities to improve care and quality of life for persons living with this disease.
References
Haye, S., Thunell, J., Joyce, G., Ferido, P., Tysinger, B., Jacobson, M., & Zissimopoulos, J. (2023). Estimates of diagnosed dementia prevalence and incidence among diverse beneficiaries in traditional Medicare and Medicare Advantage. Alzheimer’s & Dementia: Diagnosis, Assessment & Disease Monitoring, 15(3), e12472.
Jacobson, M., Ferido, P., & Zissimopoulos, J. (2023). Health care utilization before and after a dementia diagnosis in Medicare Advantage versus traditional Medicare. Journal of the American Geriatrics Society.
Zissimopoulos, J. M., Joyce, G. F., & Jacobson, M. (2023). Trends in Incident Dementia Diagnosis Before and After Medicare Risk Adjustment. JAMA Network Open, 6(12), e2347708-e2347708.
Affiliations
The USC Schaeffer Center for Health Policy and Economics researchers’ affiliations include: Schaeffer Center’s Aging and Cognition Research Program at the University of Southern California, USC’s Alzheimer’s Disease and Related Dementias Resource Center for Minority Aging Research (USC ADRD RCMAR) and the Center for Advancing Sociodemographic and Economic Study of Alzheimer’s Disease and Related Dementias (CeASES-ADRD).
Funding for this research was provided by RCMAR (P30AG043073) and CeASES ADRD (P30AG066589). Editorial support was provided by Rose Li and Associates.
Sign up for Schaeffer Center news



You must be logged in to post a comment.