What’s the latest in health policy research? The Essential Scan aims to help keep you informed on the latest research and what it means for policymakers. It is produced by the USC-Brookings Schaeffer Initiative for Health Policy, a collaboration between the Brookings Institution and the USC Schaeffer Center for Health Policy & Economics. To sign up to receive the Essential Scan straight to your inbox, sign up here.
Estimating Potential Spending on COVID-19 Care
Study by: Matthew Fiedler and Zirui Song
The disruption to the healthcare system caused by COVID-19 is having major financial consequences for providers, insurers, and patients. A new study seeks to estimate the direct cost of COVID-19 care in the United States. The authors estimate spending on COVID-19 care for scenarios in which 5 percent and 60 percent of the U.S. population is ultimately infected with the coronavirus and a range of hospitalization rates derived from New York City data. At a 5 percent infection rate, estimated COVID-19 spending ranges from half a percent to 1.0 percent of all healthcare spending, depending on the hospitalization rate. If the infection rate is 60 percent, the estimated COVID-19 spending ranges from 3.5 percent to 9.6 percent of overall healthcare spending. The authors also estimate COVID-19 spending by payer type. Based on their projections, the authors conclude that financial aid to insurers for the 2020 plan year, which industry groups have requested, would likely be a windfall to insurers. Looking ahead to 2021, the authors note that uncertainty regarding COVID-19 could lead insurers to set higher premiums for the 2021 plan year. Policies aimed at mitigating that uncertainty might be helpful, but any policies would need to be carefully designed. Full study here.
Productivity Growth in Treating a Major Chronic Health Condition
Study by: John A. Romley, Dana Goldman, Neeraj Sood, and Abe Dunn
As healthcare costs continue to take up an increasing share of the country’s GDP, productivity in care delivery has received renewed interest from insurers and policymakers. A new study adds to the literature by analyzing productivity growth for treatment of an important chronic health condition: type 2 diabetes. Researchers analyzed data from fee-for-service Medicare beneficiaries and found costs associated with treating a newly diagnosed patient decreased during the time period analyzed while health outcomes improved. Overall, researchers identified a 2.2 percent average annual improvement in productivity for this condition from 2004 to 2012, mostly from lower costs. They note that measured productivity growth in diabetes treatment exceeds recent estimates of productivity growth in acute care. These results suggest that healthcare productivity might not necessarily lag behind productivity growth in the broader economy as a whole, as previously suggested. Full study here.
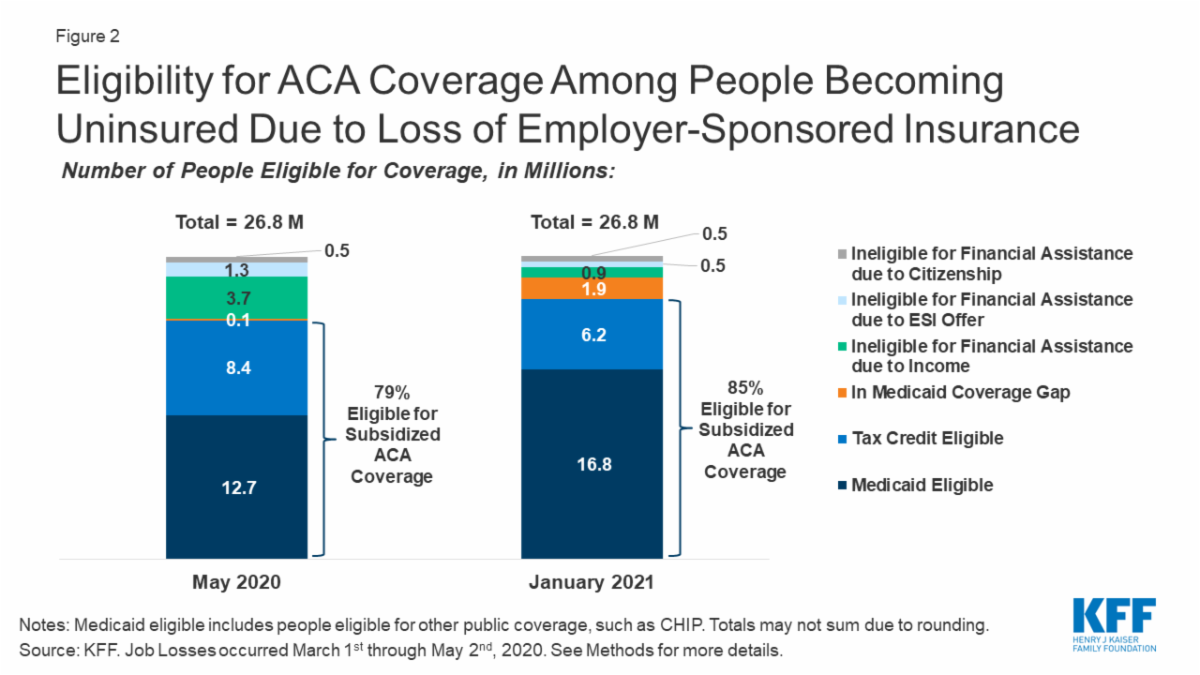
Eligibility for ACA Health Coverage Following Job Loss
Study by: Rachel Garfield, Gary Claxton, Anthony Damico, and Larry Levitt
Between March and May of 2020, more than 31 million people in America filed for unemployment insurance, but actual job loss due to the COVID-19 pandemic is likely even higher. A new analysis examines the potential loss of employer-sponsored insurance (ESI) among people in households with employment losses between March-May 2020 and estimates their eligibility for health coverage through the Affordable Care Act, including Medicaid, marketplace subsidies, and private coverage as a dependent via a parent or spouse. They find that nearly 27 million people could potentially lose ESI by May 2020. Of those, 12.7 million are eligible for Medicaid and 8.4 million are eligible for marketplace subsidies. About 5.7 million individuals who lose ESI are not eligible for publicly subsidized coverage. The analysts estimate that if those recently unemployed have not found work by January 2021 (when unemployment insurance benefits cease for most people), eligibility will increase to nearly 17 million individuals eligible for Medicaid and 6 million eligible for marketplace subsidies. They note estimates of coverage loss and eligibility vary by state, especially in regard to Medicaid access. The authors note that without the coverage protections afforded by the ACA, many more people would likely become uninsured as the country heads into a recession. Full study here.
Identifying Sources of Inefficiency in Healthcare
Study by: Amitabh Chandra and Douglas O. Staiger
There is a substantial variation in treatment rates and patient outcomes across hospitals, even after controlling for patient risk. Typically, this variation is explained in two ways: (1) some providers are delivering too much or too little of a treatment; (2) some hospitals are better at providing a specific treatment or have greater expertise and therefore deliver more of that treatment than their competitors. A new study uses econometrics to test these explanations by comparing treatment for heart attack patients. Researchers found both explanations factored into why there is variation in rates of treatment performed. Treatments performed were associated with much better patient outcomes in some hospitals than others, suggesting some variation was due to hospitals having a comparative advantage. In contrast, some amount of the variation was also due to hospitals having imperfect information and misperceiving their advantage and thus over-providing treatment. The researchers conclude that the variation in the benefits from treatment imply that a one size fits all policy, such as strict treatment guidelines, is unhelpful because hospitals with a greater comparative advantage for a treatment should use it more. Full study here.
Click here to receive The Essential Scan email.
The Essential Scan is produced by the USC-Brookings Schaeffer Initiative for Health Policy, a collaboration between the Brookings Institution and the USC Schaeffer Center for Health Policy & Economics.
You must be logged in to post a comment.