In a new Health Affairs article out today, Schaeffer Center researchers provide evidence that hospital productivity increased from 2002 to 2011, suggesting that the US health care system could be performing better than many believe. John Romley, Research Assistant Professor at the USC Schaeffer Center for Health Policy and Economics and lead author on the study observes, “The Affordable Care Act asks hospitals and other health care providers to achieve the level of productivity gains seen in the rest of the economy. In recent years, U.S. hospitals have actually managed to make that kind of improvement in treating a number of important conditions.”
Romley and his co-authors, Dana Goldman and Neeraj Sood, analyzed data of elderly Medicare beneficiaries with heart attacks, heart failure, or pneumonia over the period from 2002-2011 using a novel study design that adjusts for trends in quality of care and illness severity – factors that have not been adequately addressed in previous studies.
What Are the Key Findings?
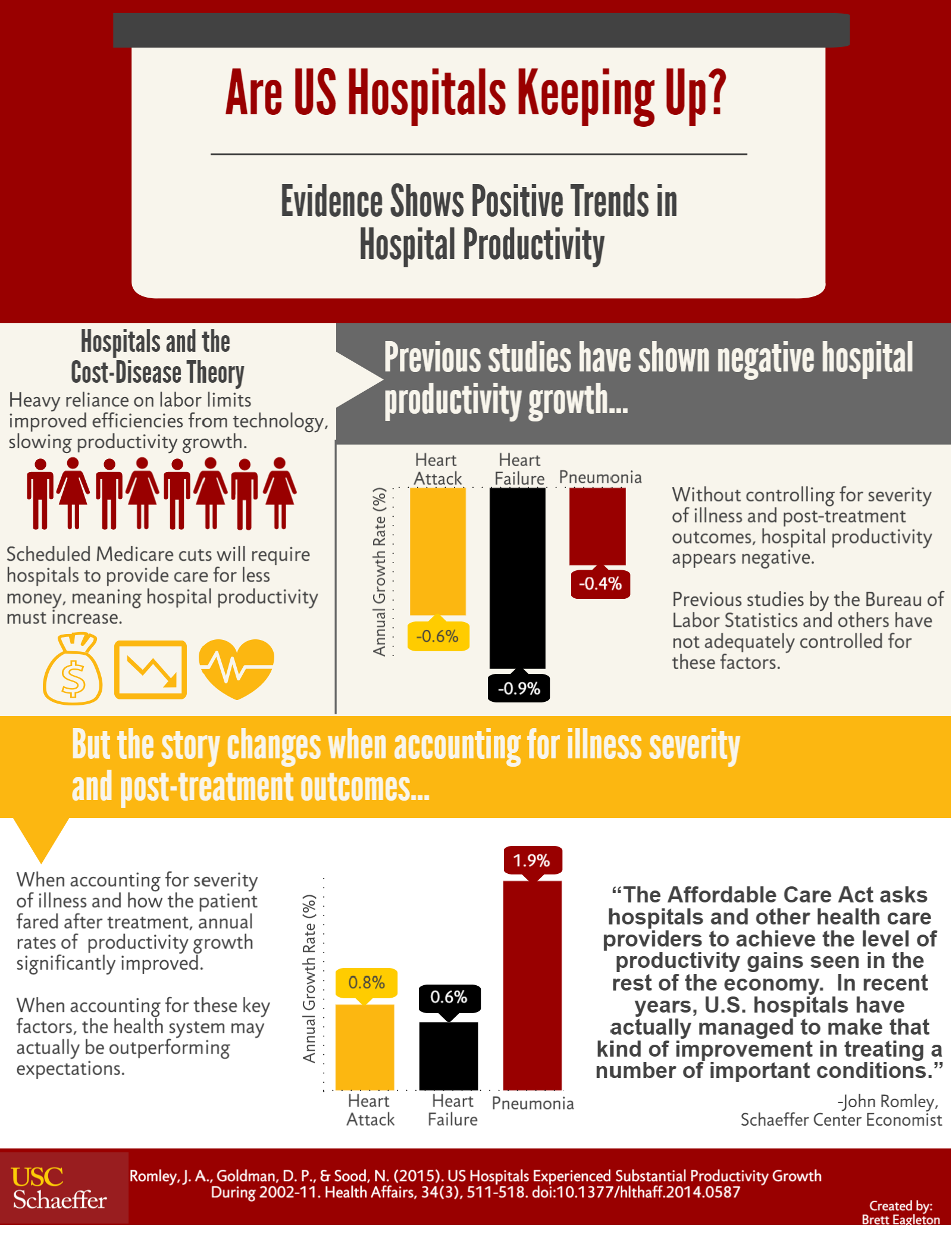
When Romley and his colleagues took quality of care and illness severity into consideration in their model, they found that the annual rates of productivity growth significantly improved to +0.78 percent per year for heart attack, +0.62 percent for heart failure, and +1.90 percent for pneumonia. These contrast with negative calculated productivity growth rates, which don’t factor in trends in the severity of patient conditions or outcomes achieved after hospitalization: -0.64 percent per year for heart attacks, -0.91 percent for heart failure, and -0.39 percent for pneumonia.
Consistent with the previous paradigm, the Bureau of Labor Statistics and health researchers have estimated that hospitals have experienced negative productivity in recent decades. This led to the argument that healthcare and service industries are affected by a so-called “cost disease,” where a heavy reliance on labor limits opportunities for cost efficiencies stemming from technological progress. The findings from this study indicate that these concerns may be misplaced.
What are the Policy Implications?
With the Affordable Care Act linking Medicare reimbursement rates to economywide productivity, some observers have questioned whether hospitals will be able to balance their budgets without compromising quality or services, if productivity grows relatively rapidly in the broader economy. Today’s study results show that this concern may be unwarranted. The findings show that productivity in the inpatient setting has improved in recent years, with its growth rate for pneumonia- which accounted for 1.1 million hospital stays in 2010- outpacing the national productivity growth rate.
“Moreover, innovative payment and delivery approaches under the ACA and among private payers may increase the incentives of hospital leaders and managers to achieve productivity gains in the future,” state the authors in the study. “Thus, quality of care need not decline even if reimbursement does not keep up with health care cost inflation.”
As the nation focuses on payment system reform, measuring productivity appropriately and effectively is increasingly important. This study demonstrates that by leveraging rich data to measure key factors like illness severity and post-discharge health outcomes, provider productivity can be properly evaluated, and our health system may actually be outperforming expectations.

You must be logged in to post a comment.