What’s the latest in health policy research? The Essential Scan, produced by the Schaeffer Initiative for Health Policy, aims to help keep you informed on the latest research and what it means for policymakers. To sign up to receive the Essential Scan straight to your inbox, sign up here.
340B Drug Pricing Program Exploited by Hospitals
Study by: Sunita Desai and J. Michael McWilliams
The 340B Drug Pricing Program offers hospitals that serve a disproportionate number of low-income patients substantial discounts on outpatient drugs while preserving their right to seek standard reimbursements from insurers. Although policymakers initially meant for the profits hospitals generated through this program to be used to expand access to care for vulnerable populations, they neglected to make this intention a strict requirement of the law and instead gave hospitals complete control over their new profits. A new study that compares hospitals eligible for the 340B program with otherwise similar hospitals finds that eligible hospitals employ 230 percent more hematologist-oncologists and 900 percent more ophthalmologists, but found no evidence that hospitals participating in the 340B program were investing more in safety-net providers or provide more care to low-income patients. These findings suggest that hospitals are acquiring more hematologist-oncologists and ophthalmologists who can administer profitable outpatient drugs in order to increase hospital revenue without fulfilling the spirit of the 340B program by using their profits to benefit low-income patients. This study highlights the potential dangers of providing inadequate oversight of even the most well intended program. Full study here.
“We need to make sure that these funds are being used for their intended purpose. This study demonstrates the original policy objectives were lost in implementation.”
-Dana P. Goldman, PhD, Leonard D. Schaeffer Director’s Chair and Distinguished Professor of Public Policy, Pharmacy and Economics, University of Southern California
Medicare Advantage Enrollees More Likely than Fee-For-Service Medicare Enrollees to Enter Lower-Quality Skilled Nursing Facilities
Study by: David J. Meyers, Vincent Mor, and Momotazur Rahman
Insurance companies that operate Medicare Advantage (MA) plans attempt to compete with traditional fee-for-service Medicare (FFS) by offering a “narrower” provider network at lower costs. However, narrowing the network of providers available to enrollees must be done carefully in order to avoid negatively affecting their access to high quality care. A new study finds that between 2012 and 2014 fewer enrollees in both lower- and higher-quality MA plans (-4.22 and -2.46 percentage points, respectively) had access to higher-quality skilled nursing facilities (SNFs) compared to FFS enrollees.They also found enrollees of lower-quality MA plans entered SNFs with higher re-hospitalization rates compared to FFS enrollees. Though the link between quality ratings and their effect on patient outcomes is difficult to quantify, these findings point to the importance of better understanding the effects of SNF decisions and network design on patient outcomes, especially as MA continues to grow in popularity. Full study here.
Community Benefit Spending by Tax-Exempt Hospitals Changed Little after ACA
Study by: Gary J. Young, Stephen Flaherty, E. David Zepeda, Simone Rauscher Singh, and Geri Rosen Cramer
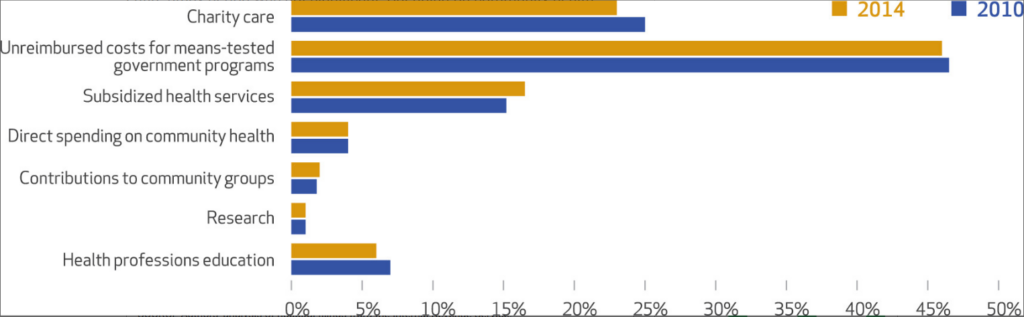
The Affordable Care Act was expected to generate positive spillover effects for low income communities by increasing community health benefit spending by tax-exempt hospitals, promoting the adoption of population health management techniques, and requiring hospitals to conduct a community health needs assessments every three years. Policymakers also hoped that by reducing the number of uninsured individuals, the demand for hospital-based charity care would fall, resulting in freed funds for hospitals to use for other types of community benefits. Using IRS data, researchers studied over two-thirds of all tax-exempt general hospitals from 2010-2014. They found that tax-exempt hospitals’ average spending on community benefits increased from 7.6 to 8.1 percent of operating expenses in the four years studied. However, this spending increase was mostly attributed to an increase in spending on patient care benefits, while spending for community health benefits remained flat throughout the study period. This study indicates that while policymakers may have intended for hospitals to play a larger role in community health management following the ACA, a more targeted approach with better aligned incentives may be required to establish the partnerships and collaborations needed for a hospital to provide effective services at the community level. Full study here.
For the Near Poor, Marketplace Plans Poor Substitute for Medicaid
Study by: Fredric Blavin, Michael Karpman, Genevieve M. Kenney, and Benjamin D. Sommers
Under the Affordable Care Act, individuals and families with incomes between 100 and 138 percent of poverty can gain coverage either through state expansion of Medicaid or through tax credits and cost sharing subsidies to use for private insurance plans available through the Marketplaces. A recent study evaluates the effectiveness of these two approaches by exploiting the differences between states that expanded Medicaid in 2014 and those that did not. The researchers find that states that expanded Medicaid had a 4.5 percent decrease in the uninsurance rate among adults with incomes between 100-138 percent FPL and that individuals who were able to enroll in Medicaid spent $344 less on out-of-pocket expenditures, $125 less on premiums, and $218 less on cost-sharing compared to individuals who enrolled in Marketplace plans each year, on average. Furthermore, the study found that Medicaid expansion was associated with a 4.1 percentage-point reduction in the probability of these near poor adults having a “high total out-of-pocket spending burden.” These results suggest that the low cost-sharing and flexible sign-up requirements associated with Medicaid could make it a more effective tool for increasing access to insurance and financial stability for the near poor than more costly and restrictive marketplace plans. Full study here.
The Essential Scan is produced by the USC-Brookings Schaeffer Initiative for Health Policy, a collaboration between the Center for Health Policy at the Brookings Institution and the USC Schaeffer Center for Health Policy & Economics.