What’s the latest in health policy research? The Essential Scan, produced by the Schaeffer Initiative for Innovation in Health Policy, aims to help keep you informed on the latest research and what it means for policymakers. To receive the Essential Scan in your inbox, sign up here.
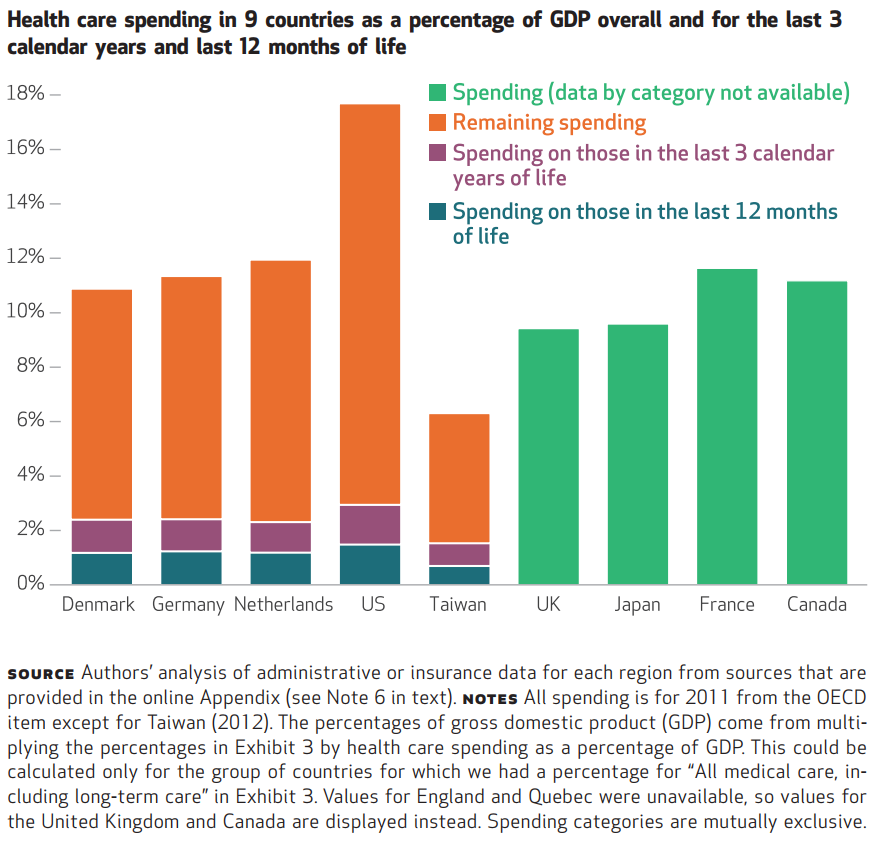
16.7 PERCENT OF TOTAL HEALTH CARE SPENDING CONSUMED IN FINAL THREE YEARS OF LIFE AMONG ELDERLY IN U.S.

Eric B. French, Jeremy McCauley, Maria Aragon, and co-authors find that health care spending among elderly Medicare beneficiaries in their last three years of life accounted for 16.7 percent of total health care spending, and 8.5 percent in the last 12 months. These shares of total spending were slightly lower than that of the other four developed countries with complete data, ranging from 10.01 – 11.20 percent in the last year and 19.40 – 24.48 percent in the last three years. However, as the U.S. has higher absolute levels of total health spending, per capita spending in the last year and three years before death was higher in the U.S. than in the other countries. These findings come in below previous estimates of last-year-of-life spending, and suggest that costliness in end-of-life care may be less a result of “last-ditch efforts” in an individual’s last year of life than it is a result of care for individuals with chronic conditions and their complications as they age. Full article here.
9 IN 10 END-OF-LIFE CAREGIVERS UNPAID; NOT SIGNIFICANTLY MORE LIKELY TO BE INSURANCE FUNDED COMPARED TO NON-END-OF LIFE CAREGIVERS DESPITE TWICE AS MANY REPORTED WEEKLY HOURS
Katherine A. Ornstein, Amy S. Kelley, Evan Bollens-Lund, and Jennifer L. Wolff find that end-of-life caregivers for elderly Medicare beneficiaries provided twice as many weekly hours of care than that of non-end-of-life caregivers, yet the elderly at the end of life were not significantly more likely to receive insurance-funded caregiving services. Expanding beyond previously disease-specific and convenience-sampled studies of caregiving, the authors used nationally representative data on the more than 900,000 elderly Medicare beneficiaries who died in 2011. These beneficiaries received caregiving support from over 2.3 million individuals, of which nearly 9 out of 10 were unpaid. As the authors note, these findings come at a time of decline in family members’ contentedness with the level of support given to their loved ones during the end of life and suggest a need for greater financial support during the end of life care period. Full article here.
POSITIVE ASSOCIATION BETWEEN HOSPICE PROFIT MARGINS AND RATES OF DISCHARGING LIVING PATIENTS, MORE RESEARCH NEEDED TO UNDERSTAND OUTCOMES
Rachel Dolin, Mark Holmes, and co-authors find a positive relationship between a hospice’s profit margins and its “live discharge” rates, and that hospices in the top third for live discharge rates were more likely to be for-profit entities and have had fewer years eligible for Medicare reimbursement than hospices in the bottom two thirds. Median length of stay in hospice care was significantly higher among the top third, at 82.0 days, compared to 61.8 days for the middle cohort and 46.5 days for the third with the lowest live discharge rates. Rather than quality, the authors point out that higher live discharge rates may be the result of other hospice- or patient-level characteristics, such as a broader initial eligibility criteria, higher levels of patient-initiated live discharge among certain groups, or based on financial considerations. The authors are skeptical of suggestions that rising live discharge rates may be a result of increased quality of care in hospices, pointing to variation across hospice types as well as prior research findings of worse outcomes among patients discharged alive compared to those that remained in hospice care until death. Given the premise of hospice care is to make terminal patients more comfortable during their last days, the findings raise concerns about recent changes to hospice payment rates that provided larger reimbursements at the beginning and end of a patient’s hospice care, and call for further study of the relationship between profit and live discharge rates in hospices. Full article here.
ADMISSION RATES TO DRUG ABUSE TREATMENT CENTERS DECLINED 32 PERCENT AMONG 18- TO 24- YEAR- OLDS FOLLOWING A MANDATE FOR DOCTORS TO USE A DRUG-MONITORING DATABASE

Dhaval M. Dave, Anca M. Grecu, and Henry Saffer find that prescription drug monitoring programs (PDMPs) have little effect without requiring physicians query the database that tracks controlled substance use prior to prescribing. Using a difference-in-differences approach to evaluate the rate of admissions to drug abuse treatment centers before and after mandatory-access PDMP implementation, the authors find mandatory-access PDMPs significantly reduce the number of adults admitted to substance abuse treatment facilities. The greatest reduction was seen among 18 – 24 year olds (32 percent decrease from prior year), followed by 25 – 44 year olds (17 percent decrease), and finally among adults older than 45 (12 percent decrease). Interestingly, the authors also find spillover effects from mandatory-access PDMPs for marijuana and cocaine. This study demonstrates efficacy of PDMPs only when accompanied by mandatory access provisions. Full article here.
2006 MASSACHUSETTS HEALTH REFORM (ROMNEYCARE) REDUCED SHORT-TERM ENROLLMENT AND OVERALL ADVERSE SELECTION
Laura F. Garabedian Dennis Ross-Degnan, Stepehn B. Soumerai, and co-authors find that the Massachusetts’ 2006 health reform mandating coverage and establishing an individual marketplace reduced the rate of disenrolling from unsubsidized insurance before 180 days by 10.35 percent and before one year by 7.50 percent. Using seven years of patient-level data from Harvard Pilgrim Health Care insurance plans, the authors find that rates of inpatient and emergency department service utilization were significantly lower but elective procedure utilization results were mixed; however, their findings indicated an overall reduction in adverse selection in the individual market. Because the Affordable Care Act (ACA) was modeled after Massachusetts’ reform, these findings bolster claims of sustainability in the unsubsidized individual ACA markets and bring to light issues of impact on utilization and health plan participation to continue observing among the ACA marketplaces. Full article here.
Editor’s Note: The Essential Scan is produced by the Schaeffer Initiative for Innovation in Health Policy, a collaboration between the Center for Health Policy at the Brookings Institution and the USC Schaeffer Center for Health Policy & Economics. To receive the Essential Scan in your inbox, sign up here.
You must be logged in to post a comment.