What’s the latest in health policy research? The Essential Scan, produced by the Schaeffer Initiative for Innovation in Health Policy, aims to help keep you informed on the latest research and what it means for policymakers. To receive the Essential Scan in your inbox, sign up here.
Medicaid patients 20 percent more likely to wait 20 minutes or more in doctor’s office than privately insured
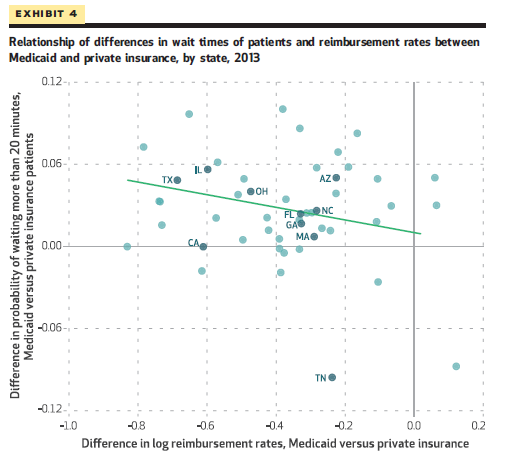
Tamar Oostrom, Liran Einav, and Amy Finkelstein find that Medicaid patients are 20 percent more likely than privately insured patients to wait 20 or more minutes for their doctor’s appointment, with half of this difference attributable to different characteristics of the practices of Medicaid patients such as practice size. Moreover, the authors find greater relative difference between Medicaid and privately insured wait times in states with lower Medicaid reimbursement rates. When exploring patient and appointment characteristics, the authors find that wait times were shorter for younger patients, morning appointments, and at larger practices. Notably, these estimates of wait times do not include time waiting inside exam room, nor the time spent waiting to schedule an appointment. These findings add non-health outcome data to the policy debate over the relationship between Medicaid reimbursement rates and Medicaid patients’ access to and quality of care. Full article here.
“In health policy, we tend to focus on how cost-sharing and copayments impact demand for services like physician office visits. But even when patients pay little or nothing – as in Medicaid – there are other, non-pecuniary factors determining who gets care. Rationing care through long wait times and low reimbursement is hardly the best strategy.”
– Dana Goldman, PhD, Director of the Schaeffer Center
Fair pricing laws reduced uninsured patients’ payments, as well as the amount of care provided
Michael Batty and Benedic Ippolito find that while state-enacted fair pricing laws, which limit how much uninsured patients may be required to pay a hospital for care, reduce uninsured patients’ prices for hospital care received by 25 to 30 percent. They find such laws also spurred hospitals to reduce the intensity and quantity of care for uninsured patients. In particular, hospitals shortened inpatient stays for uninsured patients by 7 to 8 percent in addition to reducing the number of minor therapeutic services provided to uninsured patients during a stay. Yet, the authors find no evidence that that these reductions in utilization translate to reduced quality on measures such as in-hospital mortality or 30-day readmission rates. These findings document the ways in which health care providers respond to financial incentives, and affirm the ability to realize efficiency gains within the health care system. Full article here.
High-cost Medicare patients modestly concentrated among hospitals, which are more likely to be academic medical centers and for-profit
Nancy D. Beaulieu, Karen E. Joynt, Robert Wild, and Ashish K. Jha find that while high-cost patients are modestly concentrated among hospitals and hospital referral regions, the share of total claims associated with care for high-cost patients remains high in all hospitals. Using a sample of Medicare data, high-cost patients were defined as beneficiaries whose claims totals were in the top 10 percent. The authors find that while hospitals with the greatest concentration of high-cost care had 69 percent of all Medicare claims associated with high-cost patients, the remaining hospitals still generated 51 percent of claims via high-cost patients. Hospitals with a higher concentration of high-cost patients were more likely to be academic medical centers and for-profit. These findings may support a combination of broad and targeted policy levers to address spending among high-cost patients. Full article here.
Reduced patient cost sharing for rare disease treatment spurred 181 percent increase in R&D
Toshiaki Iizuka and Gyo Uchida find that a demand-side policy to reduce patient cost sharing of drugs and devices for rare diseases increased firm-sponsored clinical trials by 181 percent, or 0.16 trials per disease per year, with greater effect in later stage clinical trials. The authors evaluate the impact of Japan’s 2009 decision to add 17 diseases to the list of those eligible to for reduced cost sharing, comparing investment in drug research toward those diseases in the following years to that of the 300 diseases added to the list in 2015. The authors also observed no increase in physician-led clinical trials following the policy change for those diseases. These findings demonstrate the potential impact demand-side policies may have in spurring rare drug research, particularly on new uses for existing drugs and devices. Full article here.
“This study provides yet another demonstration that innovation is very responsive to price changes- and it comes from Japan. There are lessons here for those who think that reducing drug prices in the United States can be done without any cost.”
– Dana Goldman, PhD, Director of the Schaeffer Center
Click here to receive The Essential Scan email.
Editor’s Note: The Essential Scan is produced by the Schaeffer Initiative for Innovation in Health Policy, a collaboration between the Center for Health Policy at the Brookings Institution and the USC Schaeffer Center for Health Policy & Economics. To receive the Essential Scan in your inbox, sign up here.