What’s the latest in health policy research? The Essential Scan, produced by the Schaeffer Initiative for Innovation in Health Policy, aims to help keep you informed on the latest research and what it means for policymakers. To receive the Essential Scan in your inbox, sign up here.
Growing gap in life expectancy by income increases gap in lifetime retirement benefits including Medicare by $130,000

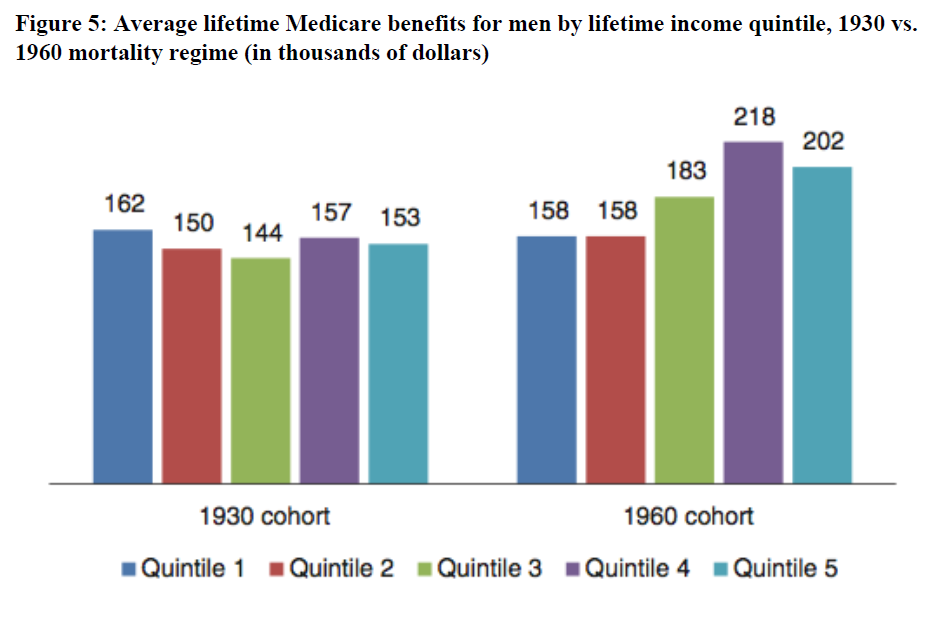
Alan J. Auerbach, Kerwin K. Charles, Courtney C. Coile, and co-authors project that, between the 1930 and 1960 birth cohorts, American men in the top earning income quintile at age 50 will gain 7 to 8 years in life expectancy, while men in the lowest-earning income quintile will gain little to nothing, thereby increasing the gap in lifetime Social Security, Medicare, and other retirement benefits between the top and bottom quintiles by a combined $130,000 (in $2009). Changes in the distribution of lifetime Medicare benefits account for a large part of the reduction in progressivity of public programs in retirement. For the 1930 birth cohort, the average lifetime Medicare benefits received by men in the lowest income quintile were 6 percent higher than in the highest income quintile. However, the 1960 birth cohort is projected to see a dramatic shift, with the lowest income quintile receiving only 78 percent of the lifetime Medicare benefits received by the top income quintile. The authors, who included Dana Goldman and Bryan Tysinger of the Schaeffer Center, simulate popular policy proposals, like changing the national retirement age, taking into account these trends. They find that though most policy proposals would make net benefits more progressive, the impact of the mortality trends tends to more than offset the policy changes. Their findings point to the significant impact the widening gap in life expectancy is having on the nature of these national programs. Full article here.
Registration mandates for prescription drug monitoring programs reduced opioid prescriptions by about 10 percent
Hefei Wen, Bruce R. Schackman, Brandon Aden, and Yuhua Bao find that state mandates from 2011 to 2014 that required physicians register with a prescription drug monitoring program (PDMP) resulted in a 9 to 10 percent decline in opioid prescriptions, as well as a reduction in spending among Medicaid enrollees as compared to non-mandate states. The authors estimate that, if adopted nationally, the Medicaid program would save over $166 million per year. Contrary to the hypothesis that an effective mandate need extend to a physician’s use of the PDMP, the authors find that mandating PDMP use was not associated with any greater reductions in either prescription numbers or spending beyond mandating registration. These findings highlight the impact PDMP-registration mandates have had on opioid prescribing rates and spending as compared to more onerous PDMP-use requirements. Full article here.
NY counties with restrictions on trans fatty acids saw fewer hospital admissions for myocardial infarction and stroke than those without
Eric J. Brandt, Rebecca Myerson, Marcelo Coca Perraillon, and Tamar S. Polonsky find that there was a 6.2 percent greater decline in hospital admissions for myocardial infarction and stroke between 2002 and 2013 in New York counties with restrictions on trans fatty acids (TFAs), as compared to those without restrictions. From 2007 to 2011, 11 New York counties implemented restrictions on TFAs that are akin to the nationwide Food and Drug Administration restriction planned for 2018. After adjusting for county characteristics, age, sex, and movement between TFA-restricted and non-restricted counties, the authors find that hospital admission for myocardial infarction declined an additional 7.8 percent in restriction counties. These findings add evidence to support the FDA’s nationwide restriction of TFAs scheduled to go into effect next year. Full article here.
Hospital admission payments comparable between Medicare FFS and Medicare Advantage, while commercial rates 89 percent higher
Jared Lane Maeda and Lyle Nelson find that commercial rates for hospital admissions are 89 percent higher than Medicare fee for service (FFS) rates ($21,433 compared to $11,354), which are largely comparable to those made by private Medicare Advantage (MA) plans. Using 2013 claims data from three large insurers and Medicare, the authors also find significant variation in the ratio between commercial and Medicare FFS rates across and within metropolitan statistical areas. Conversely, the authors found that the average hospital admission payment by MA plans was, in fact, $49 lower than the comparable average in Medicare FFS. Additionally, the authors find that readmission costs in MA do not rise with MA market share. This finding has led the Congressional Budget Office to now estimate that a premium support model would not increase payment rates as MA plan market share increases, barring any changes to out-of-network payment restrictions. Full report here.
High spending associated with 1.7 percentage point reduction in mortality risk, while high skilled nursing facility spending associated with higher mortality risk
J. Doyle Jr., John A. Graves, and Jonathan Gruber find that ambulance-transported patients treated at high-spending hospitals were associated with a modest 1.7 percentage point reduction in mortality risk as compared to those treated at lower spending hospitals. The authors use Medicare claims data from 2002 to 2012 to evaluate the relationship between hospital spending and one-year mortality rates. They find that high spending in inpatient care and home health during the 90-days following hospital admittance are modestly associated with reductions in patient one-year mortality rates while skilled nursing facility (SNF) spending is associated with a mortality increase. As the authors note, these findings call out SNF care as both a potential area to reduce spending based on the mortality outcomes observed. Yet, they also point out that further investigation is needed on the relationship between SNF care and outcomes for patients with other care needs, and to determine the extent to which SNF care is a source or marker of poor outcomes. Full article here.
Click here to receive The Essential Scan email.
Editor’s Note: The Essential Scan is produced by the Schaeffer Initiative for Innovation in Health Policy, a collaboration between the Center for Health Policy at the Brookings Institution and the USC Schaeffer Center for Health Policy & Economics. To receive the Essential Scan in your inbox, sign up here.
You must be logged in to post a comment.