Compared to patients receiving the FDA-recommended target dose of buprenorphine, patients receiving higher doses of the medication were less likely to later require emergency department services or an inpatient hospital stay, according to a new study from researchers at the RAND-USC Schaeffer Opioid Policy Tools and Information Center.
The study, published Sept. 25 in JAMA Network Open, adds to the growing evidence of the potential benefits of prescribing higher doses of buprenorphine, a highly effective medication used to treat opioid use disorder. The practice of prescribing higher doses has grown more common as the nation’s overdose epidemic has shifted from prescription opioids to especially potent synthetic opioids like fentanyl.
The U.S. Food and Drug Administration has long identified 16 milligrams as a target daily dose for patients who are prescribed buprenorphine to treat opioid use disorder. However, the researchers found that patients receiving doses above 16 milligrams, compared with patients receiving 16 milligrams, were less likely to have an inpatient or emergency hospital visit for behavioral care after starting buprenorphine treatment.
“There have been anecdotal reports about people doing better on higher doses of buprenorphine, particularly because fentanyl is a harder drug to counter – behaviorally and pharmacologically – with the target doses, but this hasn’t been fully assessed,” said study lead author Sarah Axeen, director of data and analytics at the USC Schaeffer Center for Health Policy & Economics and an assistant research professor at the Keck School of Medicine of USC. “We found that in a large sample of patients not only is there no harm of higher buprenorphine doses related to increased ED or inpatient use, but there are potential benefits.”
Researchers examined a large insurer’s database of commercial claims, including those for Medicare Advantage, between 2016 and 2021. They identified just over 35,000 patients diagnosed with an opioid use disorder who began buprenorphine treatment. The researchers sorted those patients into four groups according to their maximum sustained dose. About 43% received 8-16 milligrams, while 29% received 16-24 milligrams.
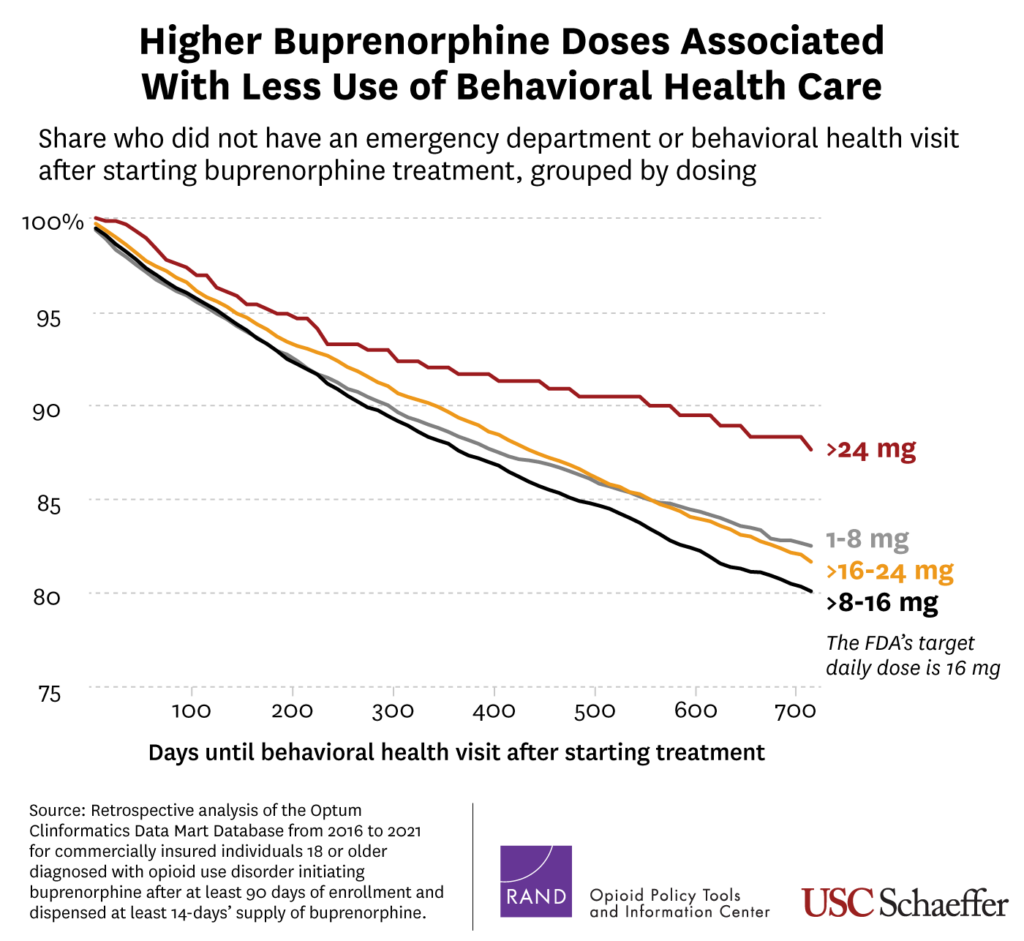
“We see some variation in how providers are prescribing, but the clustering at 16 milligrams suggests that prescribers are fairly hesitant to push that envelope at this time,” said co-author Rosalie Liccardo Pacula, a senior scholar at the Schaeffer Center and Elizabeth Garrett Chair in Health Policy, Economics & Law at the USC Price School of Public Policy. “These findings build on growing research that suggests higher doses might yield better results for some patients, particularly those who are struggling to manage symptoms from misuse of potent synthetic opioids.”
“Clinicians treating people with opioid use disorder may need to better understand the importance of finding the correct dose of buprenorphine in order to avoid more-intensive treatment in the future,” said Bradley D. Stein, a study co-author and director of the RAND-USC Schaeffer Opioid Policy Tools and Information Center. “This work provides some of the first evidence that higher doses may aid patients over the longer term.”
The study’s limitations include the absence of information about clinical symptoms and outcomes and the absence of information about non-commercially insured populations.
About the study
Other authors include Jessica S. Merlin of the University of Pittsburgh School of Medicine and Adam J. Gordon of the University of Utah School of Medicine and the VA Salt Lake City Health Care System.
Research reported in this press release was supported by the National Institute on Drug Abuse of the National Institutes of Health under award numbers P50DA046351, R01DA045800, 5K24DA056837. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
The mission of the RAND-USC Schaeffer Opioid Policy Tools and Information Center (OPTIC) is to be a national resource, fostering innovative research in opioid policy science, and developing and disseminating methods, tools, and information to the research community, policymakers, and other stakeholders. The work of the Center focuses on policy effects at multiple levels, the health care consequences of opioid misuse, and treatment access and effectiveness.
Sign up for Schaeffer Center news

You must be logged in to post a comment.