USC Schaeffer white paper finds that increasing access to obesity treatments would help save lives and reduce healthcare costs.
A new USC Schaeffer Center white paper finds the value to society of Medicare coverage for new classes of weight loss drugs would equal nearly $1 trillion over ten years.
Obesity is one of the United States’ most urgent health issues—and also one of the most treatable. Yet because Medicare and most private insurers do not cover weight-loss medications and many devices, just 1% of eligible patients receive treatments.
“Obesity is a leading risk factor for mortality in the U.S.,” says Darius Lakdawalla, director of research at the USC Schaeffer Center for Health Policy & Economics and co-author of the study. “Our modeling shows that new treatments generate substantial benefits to Medicare and its beneficiaries. Developing strategies for unlocking that value should be a priority for policymakers.” Lakdawalla is also a professor at the USC Mann School of Pharmacy & Pharmaceutical Sciences and the USC Price School of Public Policy.
Leveraging the Schaeffer Center’s Future Adult Model, an economic-demographic microsimulation model, the researchers estimated the benefits of treating Americans suffering from obesity and the cost-offsets that Medicare and society could accrue if laws were changed to allow Medicare to cover anti-obesity medications.
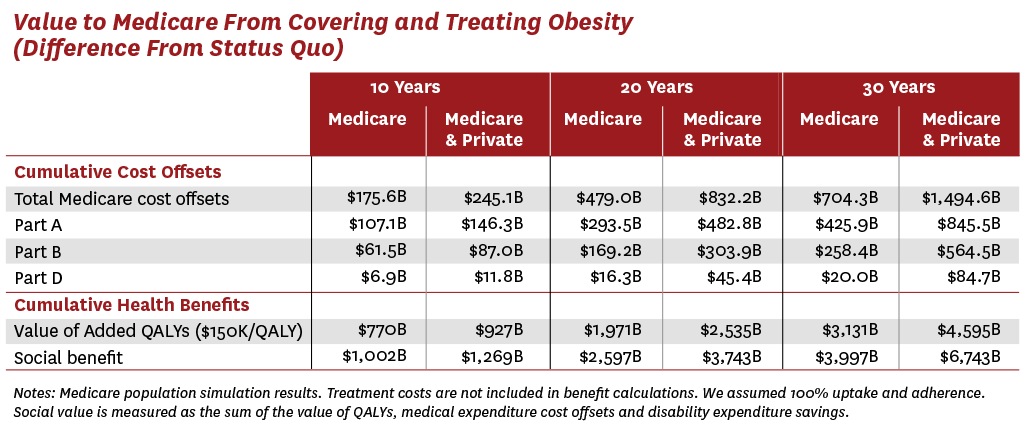
Coverage for new obesity treatments could generate approximately $175 billion in cost offsets to Medicare in the first 10 years alone. By 30 years, cost offsets to Medicare would increase to $700 billion.
The positive impacts extend beyond Medicare: society could reap as much as $100 billion per year (or $1 trillion over 10 years) of social benefit in the form of reduced healthcare spending and improvements in quality of life from reduced disability and pain if all eligible Americans were treated.
Models show the ripple effects of obesity on the healthcare system
Despite safe and effective treatments, federal law currently prohibits Medicare from paying for most forms of obesity procedures and medications. Legislation has been introduced, including the bipartisan Treat and Reduce Obesity Act, that would expand Medicare Part D’s prescription benefits to include FDA-approved drugs for chronic weight management.
Researchers discovered that most of the cost savings to Medicare—more than 60%—would flow to Medicare Part A, which covers hospital, hospice, nursing facility and home care. This could significantly help Medicare, which risks becoming insolvent by 2028.
“Because obesity is associated with many chronic conditions that significantly impact patients’ lives—and Medicare’s costs—reducing obesity rates has a ripple effect in the prevalence of other conditions,” says Alison Sexton Ward, one of the co-authors of the paper and research scientist at the USC Schaeffer Center.
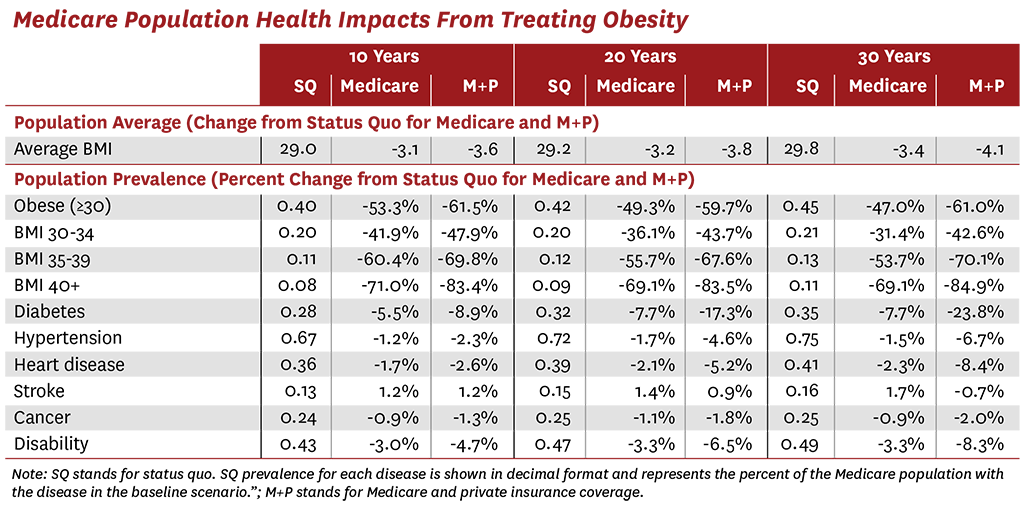
The researchers find that if all Americans eligible for obesity treatments gained access, the prevalence of obesity in the Medicare population would fall by 53% after the first decade. In addition, the researchers show that treating obesity will reduce the incidence of many related diseases, including diabetes (a 5.5% reduction in prevalence after 10 years), hypertension (1.2%) and heart disease (1.7%).
Covering obesity treatments reduces health disparities
Improving access to obesity medications could also enhance health equity, since obesity disproportionately affects Black, Hispanic and lower-income communities. More than half of the Black Medicare population has obesity and three-fourths have hypertension.
“Black and other historically marginalized communities have been disproportionately burdened by obesity,” says one of the paper’s co-authors, Bryan Tysinger, director of health policy simulation at the USC Schaeffer Center and assistant research professor at the USC Price School.
Medical breakthroughs that simplify healthcare and reduce patient effort can reduce disparities, but only if access is prioritized.
Outcomes-based pricing models would ensure access
New obesity treatments promise substantial benefits to patients if policymakers can solve the problem of how to pay for them. The researchers point to outcomes-based valuation models, including a novel pricing approach that allows for real-world evaluation of the treatments while also encouraging broad coverage.
“About half the decline in U.S. deaths from coronary heart disease over the past 50 years can be attributed to new drugs to lower cholesterol and blood pressure,” says one of the paper’s co-authors, Dana Goldman, co-director of the USC Schaeffer Center and dean of the USC Price School. “Now imagine if Congress had prohibited coverage for these lifesaving drugs. Novel pricing solutions can ensure access for all patients who would benefit from these important new anti-obesity treatments.”
PhuongGiang Nguyen also contributed to the paper. Funding for the paper was provided by the Schaeffer Center, which receives funding from foundations, government agencies, individuals, and corporations— including Eli Lilly & Company and other companies that may have interests in obesity treatments. The Future Adult Model was developed with support from the National Institute on Aging (P30AG024968).
Sign up for Schaeffer Center news




You must be logged in to post a comment.