Editor’s Note: This analysis is part of USC-Brookings Schaeffer Initiative on Health Policy, which is a partnership between Economic Studies at Brookings and the USC Schaeffer Center for Health Policy & Economics. The Initiative aims to inform the national health care debate with rigorous, evidence-based analysis leading to practical recommendations using the collaborative strengths of USC and Brookings.
In early November, the Centers for Medicare and Medicaid Services (CMS) published their final rule on implementation of Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), providing the final word on how the law will be implemented for at least its first year.
Passed and signed into law in March-April 2015 by overwhelming bipartisan majorities in the House and Senate, MACRA was a decisive move away from the former Sustainable Growth Rate (SGR) formula that beset physicians with uncertainty surrounding cuts to Medicare rates and frustrated economists by continuously deferring cost-controlling cuts.
Unlike SGR, MACRA promoted a path toward participation in Alternative Payment Models (APMs) that’s in line with goals established by the U.S. Department of Health and Human Services: to significantly increase the share of Medicare payments made to APMs and to tie payments to performance on quality and cost measures.
When HHS released its proposed rule for implementing MACRA in May, many stakeholders responded negatively to the agency’s decisions around how to qualify for Advanced APM and the participation requirements of the law’s other major payment track, the Merit-based Incentive Payment System (MIPS). Many suggested that the Advanced APM financial criteria required more risk than was necessary or reasonable to incentivize improved care, and that MIPS, as a mandatory default program, was too onerous and complex.
Given these concerns, the final rule has much for stakeholders to be happy about. It not only simplifies participation, but significantly improves upon stakeholders’ areas of concern.
Here are three important takeaways from the final rule:
- The transition period will start in 2017, with significant flexibility and lightened reporting burden in the MIPS payment track;
- The Advanced APM includes additional qualifying models, and the standards for future models’ qualification have been simplified to allow for more providers to enter into an Advanced APM earlier. This has some advantages, including exclusion from reporting in MIPS along with an automatic payment bonus of 5%; and
- Eligibility thresholds have been raised and changed, which will potentially exempt more physicians from MACRA, including those who do not have direct patient contact as well as those with low Medicare revenues.
Yet some of the most clamored-for changes among small providers are still one to two years away. For example, the minimum financial risk criteria to qualify as an Advanced APMs is lower; however, this change does more for APMs applying for qualification in future years than it does for current qualifiers, which we discuss more in detail later in the section on Advanced APMs. Another future change will be to allow solo and small group practitioners to form virtual groups, thereby easing their individual reporting burden by pooling resources and infrastructure. This leaves the comparatively lighter participation requirements of the transition year looking much like a holding pattern until these new programs come online.
This one-year delay of full implementation may not be a bad change if it avoids unduly penalizing small and independent providers while they are waiting for the fixes to come online. However, CMS should not consider the changes to Advanced APM participation complete, and should instead use the transition year to identify additional ways to more quickly develop and approve new APMs sooner rather than later.
Support a Transition Period with Increased Flexibility for Clinicians
While CMS makes clear that they are moving ahead with MACRA implementation on January 1, 2017—the date specified in the law—they established a period of transition to better support broad participation in the new program. In at least the first year, the transition period reduces participation requirements and reserves penalties virtually only for those who fail to participate at all. The final rule suspends the resource use category for the transition year by weighting its performance at zero. Furthermore, providers can begin reporting their performance on as few as one quality measure instead of six starting as late as October 2, 2017, without penalty; however, late-entrants’ positive adjustments are limited. Only providers that do not report a single measure at any point during the entire year will receive the full -4% penalty.
A temporary performance threshold in MIPS—instead of using the average or median provider score at the outset—also provides particular relief to solo and small practices in 2017, a group whose CMS-estimated performances improved dramatically under the final rule. In a significant reduction from the proposed rule, the final rule estimates that only 10% of practices with 1 – 24 clinicians, 7.4% of practices with 25 – 99 clinicians, and 1.5% of practices with 100 or more clinicians are estimated to have a penalty. CMS has not published estimated performances for 2018 and beyond, as it would be understandably difficult to fairly project providers’ performances into the second year when they have not yet even begun. However, swift and effective technical assistance to small practices will be necessary to ensure the rough parity among providers of various practice sizes remains when the MIPS performance threshold transitions to the average or median of all provider scores.
Additional Advanced APM Opportunities and Simplified Qualification
Supporting participation in the Advanced APM track under MACRA remains one of the key areas of focus among both policymakers and providers. Indeed, Advanced APMs and increasing participation in them had been the focus of Congress when passing MACRA, even though the large majority of providers would initially participate in the default pay-for-performance program MIPS. Thus, authors from Brookings submitted a comment letter in June on the proposed rule with three recommendations aimed at increasing participation in APMs among all provider types and sizes.
Qualification into the Advanced APM track grants providers not only larger long-term base payment rate increases relative to MIPS, but also the possibility of more predictable or stable financial performance when participating as a part of a larger, more organized APM entity than individually in MIPS. For independent practices in particular, APM participation also represents an opportunity to maintain the viability of their business model through shared savings.
The models projected to be granted Advanced APM qualification at the outset of MACRA in 2017, then, are:
- Comprehensive End-Stage Renal Disease Care, Two-Sided Risk;
- Comprehensive Primary Care Plus;
- Next Generation ACO Model;
- Medicare Shared Savings Program, Track 2;
- Medicare Shared Savings Program, Track 3; and
- Oncology Care Model, Two-Sided Risk (which wasopened up to participants a year early so as to enable 2017 participation).
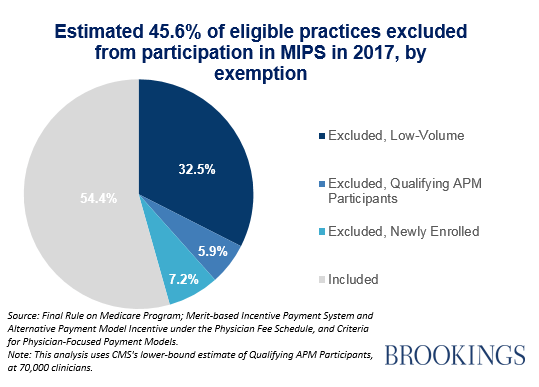
In total, CMS estimates that the qualification of these models will yield 70,000 to 120,000 (5.9% to 10.2% of those eligible) clinicians qualifying for the Advanced APM payment track.
In response to commenters, the final rule reduced the overall risk required to meet MACRA’s “nominal financial risk” standard and included a new revenue-based standard for 2017 and 2018. To meet the “nominal” standard, the final rule now only requires that APMs hold participants at risk for 3 percent of total expected expenditures, a reduction from 4 percent. In addition, the final rule will test out a revenue-based standard of 8 percent of the provider’s average estimated Medicare revenues for the first two years, which calculates financial risk according to what a provider is paid as opposed to the sum of all care costs for attributed beneficiaries. This may help small providers better assess and predictably take on risk. This revenue-based standard will stay at 8 percent for the first two performance years, with the option to increase and make it permanent thereafter.
In response to many commenters’ requests for CMS to include MSSP Track 1 in the qualifying Advanced APMs, the final rule attempted to offer a middle ground by announcing the MSSP Track 1+ model that will qualify as an Advanced APM. Prior to it becoming available to participants in 2018, more details on the model will become available. It is intended to serve as an easier “on-ramp” to taking on financial risk, and as such, the MSSP Track 1+ model would include more financial risk than Track 1 but less than either Tracks 2 or 3.
Finally, CMS opened up the opportunity for certain current models, such as the Comprehensive Care for Joint Replacement model and the Maryland All-Payer model, to adjust and reapply for Advanced APM qualification. In addition to the effect of any newly created APMs qualifying for Advanced APM status, CMS estimates that allowing existing models to recalibrate based on Advanced APM criteria and reapply for qualification will increase the number of providers qualifying for Advanced APM bonuses to between 125,000 to 250,000 in 2018.
Finally, Simplification by Exclusion
Overall, the rule estimates that over half of all Medicare physicians are estimated to be exempt from the Merit-based Incentive Payment System (MIPS) for 2017 for several different reasons, including ineligibility due to lack of patient contact, low patient or revenue volume, newly participating Medicare provider, or full or partial qualification as an Advanced APM track participant. The low volume threshold— which exempts Medicare clinicians from participating in MIPS if they care for too few or have a minimal amount of Medicare revenue—was the dominant reason clinicians were excluded from MIPS. The final rule maintained the 100 patient threshold and increased the revenue-based threshold from $10,000 to $30,000. For 2017, this new threshold excludes 32.5% of all Medicare providers.

Conclusions and Implications for Policymakers
As CMS makes clear, the final rule on MACRA is not the final word on progress in physician payment form. There is an explicit intention for the first years to be an iterative learning and development period for the program.
From a policy perspective, however, there are some important caveats and concerns:
- Despite numerous accommodations for exemptions, changes in thresholds, etc., there are still uncertainties as to whether small practices and providers will be able to navigate changes to Medicare payment independently or whether increasing pressure to consolidate practices will prove to be a more viable option.
- Several alternative payment models that are not in the “Advanced” category will be allowed to qualify for parts of MIPS (e.g., OCM measures can be submitted to qualify for parts of MIPs), yet it is not clear if this will further delay readiness for two-sided risk.
- In some cases, financial risk-taking in models that have been released prior to MACRA’s final rule exceed the nominal risk offered in the final rule. In other words, there are some models that have larger risk thresholds, exposing providers to more financial risk than the “nominal risk” called for in the final rule. For example, if a participant in the recently released Oncology Care Model chooses to participate in downside risk in 2017, they are exposed to up to 20 percent downside risk which exceeds the nominal threshold in MACRA. This leaves significant room for newly applying models to qualify as “Advanced” with much less risk than required of current proposed Advanced APMs. Utilizing this opportunity will require swift work at CMS and among interested providers to develop and propose new models, like MSSP Track 1+ and other physician-focused models.

- Implementation of MIPS, by statute, is required to be budget neutral. There will therefore be winners and losers beyond these transition years. While providers are still in the midst of evaluating and making changes to their practices for participation in MACRA’s quality program, CMS ought to work quickly to identify further opportunities to either encourage APM participation or facilitate a mechanism to identify how to thrive in the MIPS program.
- The final rule opens the door for other clinicians to also submit physician-focused payment models that would potentially pave the way for a model directly targeted to physical therapists, occupational therapists, or other clinicians that may become MIPS-eligible in future years, but the progress and foundations of payment reform for most non-physicians has not been explored. The intersection of a payment model for behavioral therapists and primary care physicians could be quite synergistic or potentially problematic.
What remains unclear is how various practices sizes will fare after the transition period in MIPS when required reporting will increase and adjustments will no longer be tied to minimum participation, but rather on comparative performance. While not available in this transition year, CMS will continue to develop the capacity to implement virtual groups in later years. Future implementation of virtual groups, as well as effective technical assistance to small provider groups, will be yet-to-be-seen components upon which many are hanging their hopes for small providers’ effective participation in MIPS.
Considering Medicare’s long-term trajectory, the support of a pipeline of alternative payment model participation—both in Advanced APMs as well as APMs in general—among all types and sizes of providers presents an opportunity to control health care costs while maintaining or improving quality. Indeed, the Medicare Shared Savings Program (MSSP) has been criticized for the lack of net savings generated in the first year of the program, analysis of the second year found that it did generate net savings, even though 95% of participants remained in MSSP Track 1 contracts where they bore no risk for losses. Further, there is evidence of spillover savings generated by ACOs into Medicare Advantage and other Medicare fee for service.
To conclude, the authors note the challenges many practicing clinicians all over the country will have navigating the implications of the MACRA final rule, which at 2,498 pages exceeds the length of the entire Affordable Care Act. Thriving in MIPS, along with flexibility to enter Advanced APMs at an earlier time, is certainly a focus point of the final rule. But whether Advanced APMs will be attractive and viable for low cost, small practices is yet to be determined. The upcoming change in administration might have an impact on the Affordable Care Act, but as you can see from the above analyses, there are important ties to MACRA which would be affected by any changes to the Medicare Delivery system reforms as well.
You must be logged in to post a comment.