USC Schaeffer Center and University of Minnesota researchers found that study participants without a college degree had even larger employment gains from lifestyle changes recommended by specialists.
Study takeaways:
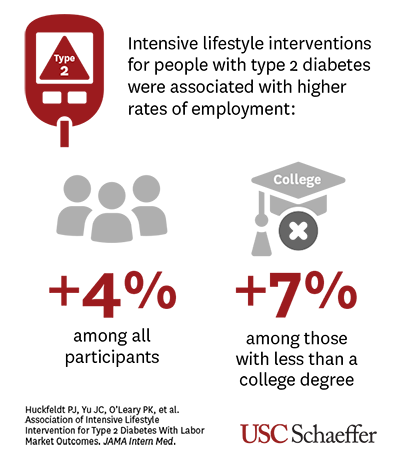
- Published in JAMA Internal Medicine, the study reveals that intensive lifestyle intervention to prevent the progression and complications of type 2 diabetes is associated with higher employment.
- Lifestyle intervention was associated with a 4% increase in employment overall, and a 7% increase among participants with less than a college degree.
- Findings suggest labor market productivity should be considered when evaluating the cost effectiveness of interventions to control chronic diseases.
Intensive lifestyle intervention for people with type 2 diabetes – including weekly counseling on diet and exercise – is associated with increased employment, according to a new study by the USC Schaeffer Center for Health Policy & Economics and the University of Minnesota School of Public Health published today in JAMA Internal Medicine.
Researchers found that employment increased 4% overall among study participants who underwent sessions with health and behavior experts who advised various lifestyle changes to prevent the progression and complications from the disease. Employment increased 7% among those with less than a college degree.
Study participants who had type 2 diabetes and who were overweight or obese were randomized to two groups. One group received an intensive lifestyle intervention including weekly one-on-one sessions with counselors, dieticians, exercise specialists, and behavioral health specialists in the first six months, decreasing to a monthly basis by the fourth year. The control group received group-based diabetes education and support sessions three times annually during the first four years, with one annual session thereafter.
The study cited prior work indicating the intensive lifestyle intervention’s effect on weight (8% reduction in the first year of the trial), physical fitness (10% increase in metabolic equivalents in the first four years of the trial), and mobility loss (48% reduction in the first four years of the trial).
Study authors noted that improvements in physical function may be more important for participants with more physically demanding jobs, who are also less likely to have a college degree.
The cohort study is among the first to link clinical trial data with Social Security Administration records to better understand the association between effective chronic disease management and labor market outcomes.
“Our study’s novel approach – linking trial data with administrative histories on employment, earnings, and disability – demonstrated the long-term economic return to better lifestyle management,” said Dana Goldman, dean and C. Erwin and Ione L. Piper chair of the USC Sol Price School of Public Policy and the co-director of the USC Schaeffer Center, who served as a principal investigator for the study.
A total of 3,091 trial participants (age 45 to 75) with type 2 diabetes who were overweight or obese were linked with Social Security data to determine whether the interventions impacted employment, earnings, and receipt of disability benefits during and after the intervention.
The research was conducted as an ancillary study to the Look AHEAD (Action for Health in Diabetes) randomized clinical trial, which analyzed whether intentional weight loss reduces cardiovascular morbidity and mortality in overweight individuals with type 2 diabetes.
“Our results contribute to the ongoing scientific inquiry into how health affects socioeconomic status and provide evidence that improving health later in life may also have positive economic benefits by extending the ability to work,” said lead author and other principal investigator Peter Huckfeldt, Vernon E. Weckwerth Professor in Healthcare Administration Leadership, University of Minnesota School of Public Health.
“These findings suggest that when evaluating interventions to manage chronic diseases, labor market productivity should be considered,” said study co-author Ann Harada, research scientist at the USC Schaeffer Center.
Additional authors included Jeffrey C. Yu, PhD, USC Schaeffer Center for Health Policy & Economics; Paul K. O’Leary, PhD, Social Security Administration; Nicholas M. Pajewski, PhD, Wake Forest University School of Medicine; Chris Frenier, PhD, University of Minnesota School of Public Health; Mark A. Espeland, PhD, Wake Forest University School of Medicine; Anne Peters, MD, USC Keck School of Medicine; Michael P. Bancks, PhD, Wake Forest University School of Medicine; and Seth A. Seabury, PhD, USC Schaeffer Center for Health Policy & Economics.
The research was supported by grants from the National Institute of Diabetes and Digestive and Kidney Diseases (R01DK107552, U01DK057136) and the National Institute on Aging (R01AG058571, U01AG073697).
Sign up for Schaeffer Center news


You must be logged in to post a comment.