Editor’s Note: This perspective was originally published on Health Affairs Forefront on March 6, 2023.
This article is part of a Health Affairs Forefront short series, “Enhancing Value By Evaluating Health Care Services.” The series discusses ways to extend the use of tools for clinical and economic evaluation beyond medical technologies to the services and procedures that account for the bulk of health care spending; the goal is to create a more robust evidence base for the effectiveness and value of health care services. The articles in the series were completed with support for the authors from the Research Consortium for Health Care Value Assessment, a partnership between Altarum and VBID Health, through a grant from the Pharmaceutical Research and Manufacturers of America (PhRMA). PhRMA extended complete independence to Altarum to select researchers and specific topics. Health Affairs retained review and editing rights.
The Inflation Reduction Act drug price provisions will establish a new Medicare Drug Price Negotiation Program whose role is to set prices for medicines in Medicare. This program was created to control costs in Medicare, yet in the policy debate ahead of its creation there was little attention paid to addressing the largest and fastest drivers of Medicare spending. A key driver of the high health care costs in the US is the overall usage of health care services, particularly spending on provider-led services in the inpatient, outpatient, and emergency department settings. Well-established economic methods such as health technology assessment (HTA) can be used to measure costs and clinical benefits of comparative services to improve the efficiency of resource allocation and minimize opportunity costs.
However, more than half of HTAs focus exclusively on new biotechnologies (for example, pharmaceuticals and medical devices), even though spending on these technologies represents less than 15 percent of total US health care expenditures. Thus, most of our HTAs are not focused on the 10 percent to 20 percent of health care expenditures spent on low value care, where the likely majority of variability in wasteful health care spending lies.
HTA methods such as comparative or cost-effectiveness and cost-benefit analyses can be used to understand, identify, and amplify the adoption of alternative services and technologies that improve the efficiency allocation of health services by ensuring that optimal value is delivered to patients more consistently. However, an optimal approach to HTA has not been uniformly decided upon in the US, and novel methods in decision analysis are emerging to fill gaps in existing methods (for example, distributional cost-effectiveness; multicriteria decision analysis).
Regardless, all parts of the health care delivery system—ranging from biotechnologies to provider-led health care services—should be held equally accountable for providing valuable services to patients. Recognizing the significant investment and infrastructure that already exists for HTA of biotechnologies, we recommend applying these concepts to all parts of the health care system. While the data and methodologies to apply HTA to medicines may be more readily apparent, there is no reason why we cannot apply the same concepts to surgeries, screenings, and other supply-sensitive procedures. We believe there is ample opportunity to expand health technology assessments today to other parts of the health system, particularly those driving cost growth.
A call to phase-out low-value services
In contrast to pharmaceutical technologies, health care services are often not subject to the same rigor of HTA to gain market access. The lack of hurdles to gain market access or remain accessible for providers to use creates a dearth in data on clinical benefits of medical services that otherwise would flow directly into value estimations.
The USC Schaeffer Center-Aspen Institute has called for more focus in health economics on examining the value defects in health care services in addition to biotechnologies. It may be that applying HTA with a balanced plan to examine biotechnologies and health care services would mean reduced reimbursements for low-value health care services that lead to phasing out spending on wasteful health care.
The US has not yet sought to leverage existing data to assess the value of costly and commonly used health care services. The US should use available data to make a sound value story and fill the gaps in economic evidence, while acknowledging and documenting information limitations. Effectiveness data in particular pose a challenge for health services interventions. Challenges include defining and distinguishing effectiveness from broader concepts of quality of care; measuring health outcomes that matter most to patients; designing effectiveness studies when faced with non-random allocation of groups in clinical practice; measurement challenges based on existing administrative claims and electronic medical record data; and a lack of understanding of the full cycle of care from a patient perspective.
While observational data sources have measurement limitations, they provide a good starting point.
Constant Contact Subscribe Form
Leveraging existing literature and real-word data should be the first step in driving evidence on value of health care services. We recommend a broader set of goals to be adopted with the aim of reducing wasteful health care spending:
- Synthesize and evaluate existing evidence on health care services to inform opportunities to identify low-value care or determine where additional research is needed;
- Develop a research agenda to prioritize disease areas and intervention types for value-evidence generation based on assessment of current evidence, costs, equity, and patient-need considerations, and offer guidance on methods and measurement issues;
- Identify barriers to generating HTA evidence on health care services and design a plan to invest in more robust data generation on costs and clinical effectiveness of non-technology Interventions (for example, surgeries or other procedures); and
- Conduct systematic HTA for priority health care services and use these data to identify opportunities to generate system and patient savings.
Leveraging available evidence to phase-out value defects
A roadmap to high-value care includes a collective purpose for the use of evidence for the economic evaluation of health care services (for example, supply-sensitive services, diagnostics, and procedures largely induced by providers). Our call for a smarter research roadmap recognizes large gaps in existing data but also aims to leverage available data on costs and clinical benefits, critically assess current measurement approaches, and apply a framework for organizing the available data to answer questions for health care services.
Understanding that waste and low-value care exists in health care services is useful information but does not help us identify how to correct the issue. To detect where low-value care exists, we can use the value defects framework developed by Pronovost and colleagues. We can then seek out low-value care options that are sources of wasteful spending and look at the available evidence to reverse trends in overspending for fixed or inferior gains in clinical benefits. For instance, David Dietz and colleagues used the defects in value framework to estimate the US cost per year for defects in value for colorectal surgery. Using this momentum, health service researchers should extend this work to more varied examples of health care services to better understand where wasteful spending lies throughout provider-led services.
The latter point is endemic in the field of health economics, where to date few HTAs have looked at important questions regarding inefficient spending on low-value care options with respect to biotechnology. More HTAs in the future should apply to health care services to inform decision makers about phasing out low-value service offerings. Since the literature on the economic value of health care services does not exist or is outdated, even though such offerings are currently reimbursed, we have a new opportunity to examine the cost-effectiveness of these services.
Evidence is needed on clinical and economic benefits—particularly including the cost of the intervention, cost of the alternative(s), downstream consequences on health and future use—to help assess value among various patient populations. Unlike the costs of most other goods and services, the costs of interventions in the health care services sector are quite opaque despite the rollout of government programs such as the Centers for Medicare and Medicaid Services’ Hospital Compare. In particular, there is often little transparency in the true cost of services delivered in a hospital setting despite recent rulemaking aimed at expanding hospital price transparency. The cost of health care services can be challenging to specify in particular given our extensive knowledge of small area cost variation.
Regardless, there is available evidence that can identify value defects and their costs across a variety of disease states (exhibit 1). This level of evidence should be enough to justify reduce spending in these areas.
Exhibit 1: Examples of defects in value and US cost burden for disease states
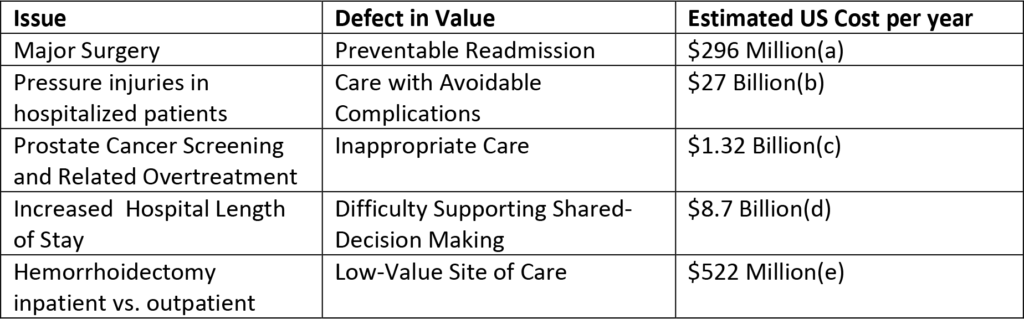
Sources: aBrown CS, Montgomery JR, Neiman PU, Wakam GK, Tsai TC, Dimick JB, et al. Assessment of potentially preventable hospital readmissions after major surgery and association with public vs private health insurance and comorbidities. JAMA Netw Open. 2021;4(4):e215503. bPadula WV, Delarmente BA. The national cost of hospital-acquired pressure injuries in the United States. Int Wound J. 2019;16(3):634-40. cAizer AA, Gu X, Chen M-H, Choueiri TK, Martin NE, Efstathiou JA, et al. Cost implications and complications of overtreatment of low-risk prostate cancer in the United States. J Natl Compr Canc Netw. 2015;13(1):61-8. dTak HJ, Ruhnke GW, Meltzer DO. Association of patient preferences for participation in decision making with length of stay and costs among hospitalized patients. JAMA Intern Med. 2013;173(13):1195-205. eDietz DW, Padula WV, Zheng H, Pronovost PJ. Costs of defects in surgical care: a call to eliminate defects in value. NEJM Catalyst. 2021 Nov 3 [cited 2023 Feb 21].
Exhibit 1 illustrates opportunities to reduce spending on low-value care across disease types. Billions of dollars are spent every year over preventable readmissions, avoidable complications, inappropriate care, difficulty in shared decision making, and care at low-value sites. While the immediate financial burden of low-value care often falls on the system or the payers, patients have the most to lose through increased out-of-pocket payments and decreased clinical benefits.
Summing up
Using HTA across the spectrum of health care delivery—from services to biotechnologies—could curb some of the $1 trillion in spending on defects in value in the US. Existing clinical literature can be leveraged to generate value evidence that leads to phasing out low-value care alternatives, as well as preserving care that offers value to select groups of individuals. The framework Peter Pronovost and colleagues coined as “defects in value” provides a way to prioritize how to identify low-value care across all disease states. Analytically speaking, this is straightforward for health economists to achieve, but the challenge will then be to phase-out what we know inhibits performance to move toward more high-value care in the US.
Authors’ note
William Padula and Brett McQueen serve as consultants for Stage Analytics.
Padula, W., Reid, N., and R.B. McQueen (2023). Addressing Value Defects From Wasteful Services Through Health Technology Assessment. Health Affairs Forefront.
10.1377/forefront.20230303.818111
Copyright © [2023] Health Affairs by Project HOPE – The People-to-People Health Foundation, Inc.



You must be logged in to post a comment.