Editor’s Note: The following is a testimony delivered by Rosalie Liccardo Pacula to the Committee on Health and Human Services, Florida House of Representatives on December 11, 2019. More information about the hearing can be found here. The opinions and conclusions expressed in this testimony are the author’s alone and should not be interpreted as representing those of the University of Southern California, RAND’s Drug Policy Research Center, NBER, ISSDP, NIH or any other sponsors of Dr. Pacula’s research.
Chairwoman Button, Vice-Chairman Plasencia, and other distinguished members of the Health Quality Subcommittee, thank you very much for the opportunity to testify before you today. I am currently an endowed chair, Full Professor in the Department of Health Policy & Management within the Sol Price School of Public Policy at the University of Southern California teaching health economics and health policy. I am also a Senior Fellow in the USC Leonard D. Schaeffer Center for Health Policy & Economics, Research Associate at the National Bureau of Economic Research (NBER), and current President of the International Society for the Study of Drug Policy (ISSDP). Before moving to USC, I served as co-Director of the RAND Corporation’s Drug Policy Research Center for 15 years, a role that had me engaging with numerous states’ policy makers and Health Canada about decriminalization, medical cannabis regimes, and recreational cannabis policies. Finally, I have been the recipient of numerous NIH grants over the past 20 years, evaluating variation in cannabis policies across states and studying their impact on criminal justice and public health outcomes. It is because of this experience I have been asked to speak to you about the likely impacts of recreational marijuana in Florida and potential marijuana regulatory structures that might be effective at minimizing potential harm.
Let me begin by saying that states, and countries for that matter, have different objectives when making the determination to legalize cannabis for adult-use (or what I will be referring to as “recreational purposes”). Some do so because they are trying to reduce the criminal justice costs imposed by prohibition, some because they want to get rid of the black market, some because they think it is a more effective way of reducing youth access and use, and others because they see that it is an attractive way of generating new tax revenue and creating jobs. The justifications provided are usually some combination of those just mentioned, and occasionally a few others, but it is the primary stated purposes – whatever they are – that are most important for determining the next two big decisions legislative bodies have to make, which are: (1) how to set up a regulatory structure to meet those objectives, and (2) with whom will the regulatory authority and oversight primarily lay. There is no one correct answer to either of these questions; the answers are necessarily and importantly tied to the primary stated purposes for changing the law in the first place. That said, if public health objectives are not a major consideration, then regulatory structures set up by the state might be insufficient to manage the risk or mitigate known public health harms associated with cannabis legalization.
What specific public health harms am I referring to? The research has pretty clearly demonstrated the following known public health risks: increases in adult use, increases in frequency of use and daily near daily use, increases in cannabis use disorder and dependence, increases in impaired driving, increases in use among pregnant and/or nursing women, increases in acute psychosis and ED visits associated with over exposure to THC among adults and children, increases in use of cannabis with nicotine (through blunts and vaping), and most recently increases in rates of vaping and dabbing, particularly among youth (Hall et al., 2019; Knapp et al., 2019; Tormohlen et al., 2019; Smart and Pacula, 2019; Wang et al., 2018; Meich et al., 2017; National Academies of Science, 2017; Volkow et al., 2017; Hall and Lynskey, 2016; Wen et al., 2015) . And while the list I just mentioned is focused on harms, that is not to imply that there are no known health benefits of cannabis or benefits from legalization. That is not the case. Nonetheless, many state jurisdictions in the U.S. have moved forward with liberalization policies ignoring the potential health risks, forgetting that (1) some of the standard quality control and product testing done on agricultural products, food and medicine to protect patients and consumers are done by the federal government; and (2) financing and support of compliance checks has also been paid for, or augmented, with federal support. In part this occurred because calls for policy liberalization have gone ahead of the science on risks; the public and policy makers both assumed the lack of rigorous science showing harm was indicative that there was no such harm, and this mindset was strongly encouraged by the budding cannabis industry. I believe jurisdictions can and should do a better job of balancing the benefits and harms of cannabis liberalization policy.
As I, and my colleagues, have written extensively on the public health impacts of cannabis liberalization policy, I will not provide a comprehensive review of them all here as part of my opening statement, although I am more than happy to answer specific questions about the literature. I strongly encourage those interested in thorough reviews on the topic to read the following studies: Smart & Pacula (2019); Hall et al. (2019), Hall and Lynskey (2016), and National Academies of Science (2017). There are, however, three specific public health impacts I would like to raise now in my opening comments because the ability to mitigate them are closely tied to key regulatory decisions that the Florida state legislature could make if considering forms of legalization for adult use, and hence serve as useful examples. They are (1) the rising trends in daily and near daily users; (2) the increases in emergency department visits, hospitalization and urgent care utilization; and (3) the rise in cannabis use among pregnant and nursing mothers. Let me discuss each of these briefly now.
- Rising trends in daily and near daily users.
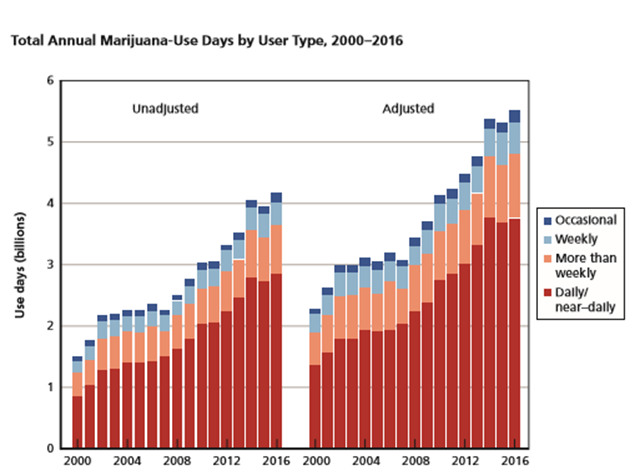
Evidence from a recent report my RAND colleagues did for the Office of National Drug Control Policy (shown in Figure 1) demonstrates two important findings about past year cannabis users (Midgette et al., 2019). First, regardless of the year in which consumption is measured, and they looked at consumption from 2000 through 2016, daily and near daily users represent at least 75% of all use days in any given year. Second, the number of use days has grown substantially across all types of past year users since 2000, with daily and near daily consumers increasing their number of use days the most substantially from just under 1.4 billion to over 3.5 billion use days. Evidence from a variety of sources using more sophisticated statistical techniques show that recent cannabis liberalization policies adopting commercialized systems have led to increases in the number of daily or near daily users as well as higher rates of cannabis use disorder (Mauro et al., 2019; Hasin et al., 2017; Wen et al. 2015). Why is this? For-profit commercialized industries make their profit by selling their commodities – whether it is alcohol, tobacco, coffee, or sugary drinks – to its most frequent consumers, which in the case of cannabis are daily and near daily users. If the goal of the state legislature is to create a market that encourages more moderate use of cannabis, with less risk of abuse and dependence, then a regulatory form of the market that does not explicitly incentivize the industry to increase sales by developing more daily and near daily users is likely to be preferable (Smart and Pacula, 2019; Caulkins 2019). As we have described in our report to the Vermont Legislature (Caulkins et al., 2015) there are a variety of alternative models to choose from, including government monopolies, non-profits, or public benefit corporations that I would be happy to discus in the Q&A.
Figure 1: Total Annual Cannabis-Use Days by Type of User, 2000-2016
- Rising trends in cannabis-involve emergency department visits, hospitalizations, and urgent care visits in liberalizing states.
There have been a series of studies showing a substantial increase in cannabis-related emergency department visits, hospitalizations, and urgent care visits throughout the U.S. among both adults (Shen et al., 2019; Zhu et al., 2016) and children (Shen et al., 2019), with statistically significant increases in states and/or locations with more liberal cannabis policies or access (Wang et al., 2018; Shi 2017; Mair et al., 2015). Looking at trends in Colorado using readily available data from the Colorado Hospital Association, the prevalence of hospitalizations for marijuana exposure in patients aged 9 years and older doubled after the legalization of medical marijuana (from 15 per 100,000 hospitalizations prior to 2010 to 28 per 100,000 for the period 2010-2013) (Kim and Monte, 2016).ED visits also nearly doubled after the legalization of recreational marijuana (from 22 per 100,00 from 2010-2013 to 38 per 100,000 from 2014-2016) (Kim and Monte, 2016). Unintentional pediatric exposures have increased substantially in Colorado as well, both with the legalization of medical cannabis (Wang et al., 2016) and then again when the state legalized cannabis for adult use (Wang et al., 2018). Research from Colorado suggests that the most common cannabis-related emergency room visits are from pediatric ingestion, acute intoxication, cannabis hyperemesis syndrome (uncontrolled vomiting), acute psychosis, and butane hash oil burns (Kim and Monte, 2016; Heard et al., 2017).
Figure 2: National Trends in Cannabis-Involved ED visits in the United States, 2006-2014
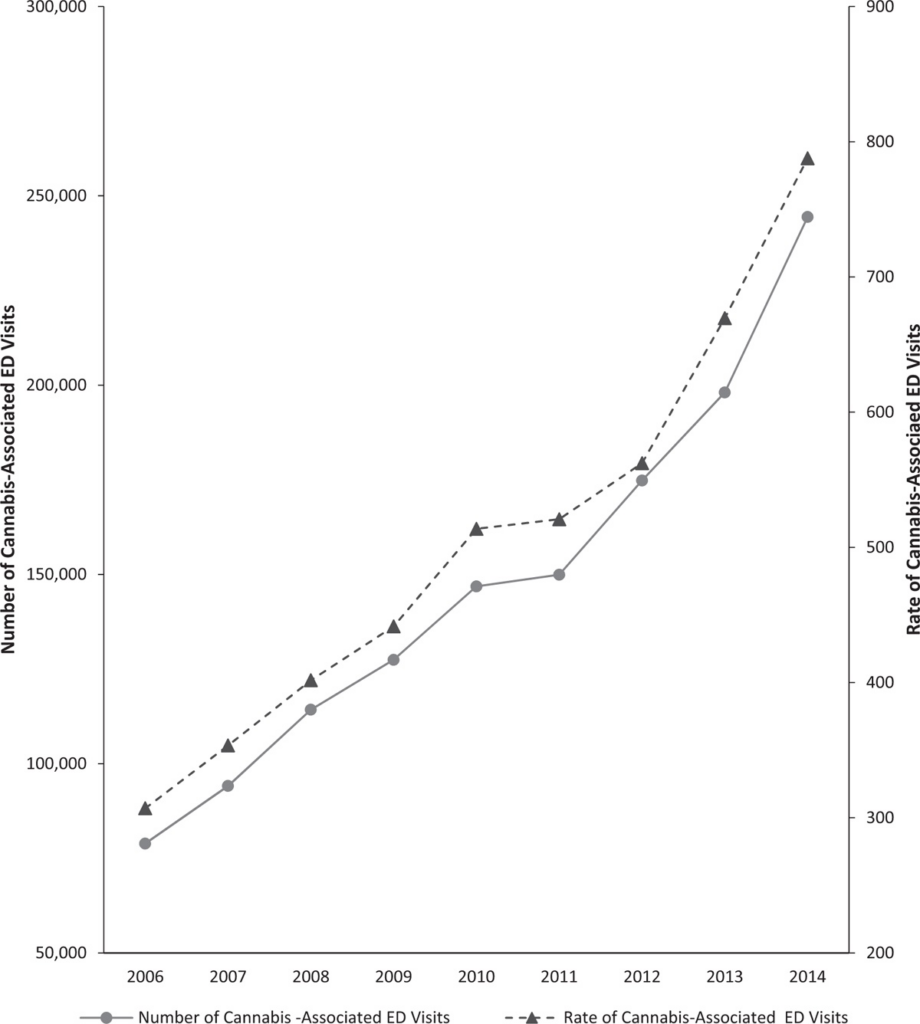
It is important to note the evidence of additional impacts of these harms transitioning from a medical cannabis system to a recreational cannabis system. Exposure to certain segments of at-risk populations grows as the market transitions from medicalization to full adult-use legalization. It is my belief that some of this exposure can be reduced through more effective regulation. In particular, the lack of attention to new product innovation by the industry, the types of products that are being developed that are either easily mistaken for non-cannabis products, and the products that are clearly targeting youth users (e.g. pot-tarts), is a major flaw of most state regulatory agencies. Consumption of edibles and extracts (oils, vape cartridges and concentrates) are much higher in recreational markets than even medical markets (Firth et al., 2019; Smart et al., 2017; Borodovsky et al., 2017) and most legalizing markets show greatest growth in extracts (Firth et al., 2019). These products have substantially higher average potencies (60-80% THC) than those of dried flower (20-30%).
While most states have rules now that suggest no candies or products that may be appealing to children, they have not yet dedicated sufficient resources to monitoring and aggressively penalizing retailers and/or producers who have products sold on the internet and shipped to residents in their state and/or sold in brick-and-mortar stores, but they could. They have also paid little attention to the growing vaping trend among youth (Borodovsky et al., 2017; Meich et al., 2017), of both nicotine and cannabis, and thus miss one of the core target audiences of the industry for these innovative vaping products. Lack of state regulatory resources to monitor products being made available on the market, ensuring proper testing by truly independent labs with experience testing these sorts of products, and proactively restricting high potency waxes, oils and the like from the market are in my mind major omissions of current state regulatory efforts. Whether it is inexperienced exposure to a high-potency cannabis-infused gummy, cookie, or soda or regular use of high potency vaping products, the health harms caused by these products are becoming clearer, and state regulatory agencies can and should do more to reduce the risks.
- Increasing use during pregnancy and while nursing.
Marijuana is highly lipid soluble and therefore crosses the placenta and blood-brain barrier easily accumulating in fetal tissues, particularly the brain (Kim et al, 2018). It can also be transferred to newborns through breastmilk (Bertrand et al., 2018). Most published studies I am aware of study consequences including increased rates of stillbirth (Varner et al., 2014) , low-birthweight (National Academy of Sciences, 2017; Crume et al. 2017), and possibly greater risk of being placed in a neonatal intensive care unit following birth (Gunn et al., 2016), although findings are a bit mixed on this last result (Crume et al., 2017). Relevant work examining longer term cognitive impairment is ongoing but marijuana use is associated with a number of neurocognitive vulnerabilities in children and adolescents (NIDA, 2019; Gunn et al., 2016). There is widespread agreement within the medical and scientific community that use of any cannabinoid during pregnancy and while nursing is not recommended and should be discouraged (Committee for Obstetric Practice, 2017; Volkow et al., 2017).
Yet, trends in cannabis use while pregnant, albeit generally low, are clearly increasing (Agrawal et al., 2019; Brown et al., 2017), with rates of use higher in liberalized states (Young-Wolff et al., 2018) and specifically among women between the ages of 18-25 (Young-Wolff et al., 2019; Agrawal et al., 2019). What is particularly discouraging about this trend is that this increase in cannabis use during pregnancy is happening at the same time we are seeing decreasing rates of alcohol and tobacco use during pregnancy (Agrawal et al., 2019). Pregnant women report cannabis use to self-treat nausea, anxiety, depression and vomiting (Young-Wolff et al., 2018 Mark et al., 2017), and it is clear that women experiencing vomiting and nausea during the first trimester of pregnancy are significantly more likely to report cannabis use (see Figure 3).
Figure 3: Rising Self-Reported Rates in Cannabis use During the First Trimester of Pregnancy in California
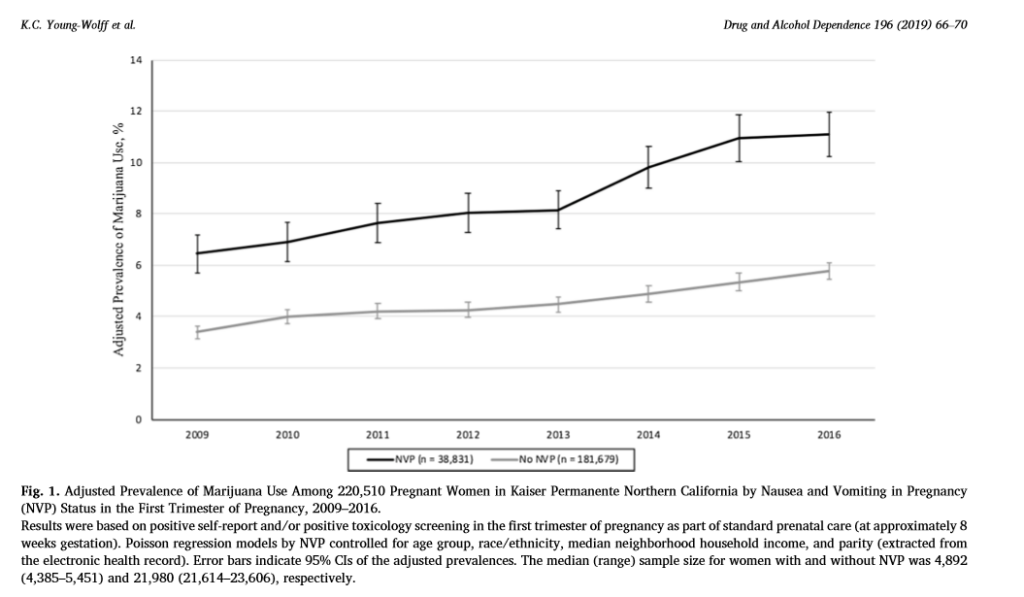
A recent important study showed that when a caller contacted 400 randomly selected cannabis stores in the state of Colorado pretending to be nauseous from the first trimester of pregnancy, the majority of dispensaries – 69% – recommended cannabis products for morning sickness (Dickson et al., 2018). Medical and recreational dispensaries were both more likely to recommend cannabis use than not to the caller (Dickson et al., 2018).
Clearly, dispensaries should not be the place where people get their information on the potential health benefits or harms of cannabis, unless those dispensaries have a board-certified pharmacist who is knowledgeable about the products. To date, only three out of 34+ states with medical cannabis laws have a model requiring pharmacy consultation from a board-certified pharmacist in their state medical program: Minnesota, Connecticut and New York. A recent study done in Minnesota demonstrated that even pharmacists reported little knowledge about the products and felt inadequately trained in cannabis pharmacology to know what to recommend to patients (Hwang et al., 2016). Without such a resource, consumers and patients rely on other employees of the dispensaries.
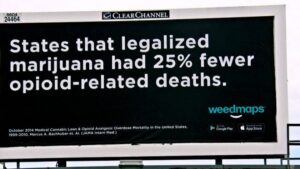
There are at least two ways state regulation could help manage this unfortunate problem. First, states could adopt significant penalties for the communication of inaccurate or scientifically refutable health claims made by the cannabis industry and/or any employee of the industry and allocate money generated from legalization to aggressively check for compliance. Second, states (along with the appropriate medical and pharmacy boards) can and should be responsible for developing the content of information used in training dispensary personnel and the general public on the risks and known benefits of particular cannabinoids for specific populations as well as the doses used in studies that evaluate harms versus the doses observed in legal markets (by product type and mode of administration). If training content and implementation is left to the cannabis industry, and not an objective health agency, it cannot be guaranteed that employees will be educated on the true science, and hence nor will the consumer. As can be seen by the real examples shown in Figure 4, the industry has already demonstrated that it is not truly conveying appropriate public health messages in its communications about cannabis to the public, so why should we believe they would do a better job training employees?
Figure 4: Exhibits of the Cannabis Industry and Cannabis Advocacy Groups Educating the Public on Perceived Cannabis Benefits

Each of the three examples I just mentioned – the increases in daily and near daily users, the rising incidence of ED visits, hospitalizations and acute care cases, and finally rising rates of use during pregnancy and nursing- represent genuine public health concerns that could lead to real short and long term costs for the state. With each of these examples I have attempted to provide examples of the ways that states could adopt more aggressive regulatory efforts, and hopefully made the case for why such a role is necessary. Cannabis is a complex group of products, not a single product. It is sold in a variety of different forms with different modes of ingestion targeting different types of users. It is a product for which (1) standardized testing- of the cultivated plant, the processed oils, and the infused products – has not yet firmly established, (2) impairment is difficult to measure, but (3) over exposure at point of use is a legitimate concern due to factors beyond just poor or inaccurate labeling.
All jurisdictions that have legalized thus far tend to move forward with the key authority and power resting in a single agency that tends to reflect the primary concern and purpose of the law (e.g. Department of Revenue, Department of Health, Department of Agriculture, etc). Some states attempt to coordinate efforts across agencies, but each individual agency tends to adopt strategies reflective of their primary goal, not the broad goals reflected by an electorate or legislatures. They also approach the objective of regulating these markets (licensing, oversight, testing, etc) using the usual tools available to them, forgetting that much of the regulatory authority and testing of the crops we grow, the plants and food we produce and sell, the medicines we regulate, involve coordinated efforts with Federal government agencies that – because of federal prohibition – will play no role in the cannabis industry.
Let me conclude by simply stating that states cannot regulate cannabis like alcohol or tobacco, as they do not have their federal partner to fall back on for many of the non-traditional state regulatory roles. As such, states have to dedicate more resources and attention to regulation of a legal cannabis market than they do either of these other products. They need to be more aggressive in testing and monitoring the quality of products and type of products sold by the industry to ensure safe products are being made available to consumers, and persistently check the compliance of the industry with these regulations. This costs money – money that would be available through the legal system, but money that to this point has been insufficiently allocated in other legalizing jurisdictions. Alternatively, states could choose to open markets up slowly, restricting certain products from the recreational market until such time as the state can ensure proper testing, labeling and compliance checks for those who sell them. That is, in fact, the course that Canada recently took with its own policy.
With that I would like to open it up to questions.
References
Agrawal, A., Rogers, C. E., Lessov-Schlaggar, C. N., Carter, E. B., Lenze, S. N., & Grucza, R. A. (2019). “Alcohol, cigarette, and cannabis use between 2002 and 2016 in pregnant women from a nationally representative sample.” JAMA Pediatrics, 173(1), 95-96.
Borodovsky, J. T., Lee, D. C., Crosier, B. S., Gabrielli, J. L., Sargent, J. D. and A.J. Budney (2017). U.S. Cannabis legalization and use of vaping and edible products among youth. Drug and Alcohol Dependence 177: 299–306.
Health Canada (2018). Canadian Cannabis survey: 2018 summary. Available at: https:// www.canada.ca/en/services/health/publications/drugs-health-products/canadiancannabis-survey-2018-summary.html.
Caulkins, J. (2019). Legalising drugs prudently: The importance of incentives and values. Journal of Illicit Economies and Development, 1(3).
Caulkins JC, Kilmer B, Kleiman MAR, MacCoun RJ, Midgette G, Oglesby P, Pacula RL and PH Reuter. (2015). Considering Marijuana Legalization Insights for Vermont and Other Jurisdictions, RAND Report RR- 864. Santa Monica, CA, January 2015.
Committee on Obstetric Practice. (2017). “Committee opinion No. 722: marijuana use during pregnancy and lactation.” Obstetrics and gynecology, 130(4), e205.
Crume, T. L., Juhl, A. L., Brooks-Russell, A., Hall, K. E., Wymore, E., & Borgelt, L. M. (2018). “Cannabis use during the perinatal period in a state with legalized recreational and medical marijuana: the association between maternal characteristics, breastfeeding patterns, and neonatal outcomes.” The Journal of Pediatrics, 197, 90-96.
English DR, Hulse GK, Milne E, Holman CB, and CI Bower (1997). “Maternal cannabis use and birth weight: a met-analysis.” Addiction 92: 1153-1160.
Firth, C. L., Davenport, S., Smart, R., and J.A. Dilley (2019). “How high: Differences in the developments of cannabis markets in two legalized states.” The International Journal on Drug Policy, 75, 102611.
Gunn JKL, Rosales CB, Center KE, et al. (2016). “Prenatal exposure to cannabis and maternal and child health outcomes: a systematic review and meta-analysis.” BMJ Open 6 (4).
Hall, W., & Lynskey, M. (2016). Evaluating the public health impacts of legalizing recreational cannabis use in the United States. Addiction, 111(10), 1764-1773.
Hall W., Stepanovic D, Caulkins J, Lynskey M, Leung J., Campbell G and L Degenhardt (2019). “Public health implications of legalizing the production and sale of cannabis for medicinal and recreational use” The Lancet 394(10208), 1580-1590.
Hasin, D. S., Sarvet, A. L., Cerdá, M., Keyes, K. M., Stohl, M., Galea, S., & Wall, M. M. (2017). “US adult illicit cannabis use, cannabis use disorder, and medical marijuana laws: 1991-1992 to 2012-2013.” JAMA Psychiatry, 74(6), 579-588.
Hwang, J., Arneson, T. and W.S. Peter (2016). “Minnesota pharmacists and medical cannabis: a survey of knowledge, concerns, and interest prior to program launch”. Pharmacy and Therapeutics, 41(11), 716.
Heard, K., Marlin, M. B., Nappe, T., & Hoyte, C. O. (2017). “Common marijuana-related cases encountered in the emergency department.” American Journal of Health-System Pharmacy, 74(22), 1904-1908.
Kim J, de Castro A, Lendoiro E, Cruz-Landeira A, Lopez-Rivadulla M, and M Concheiro. (2018). “Detection of in utero cannabis exposure by umbilical cord analysis”. Drug Testing and Analysis. 10(4): 636-643.
Kim, H. S., & Monte, A. A. (2016). “Colorado cannabis legalization and its effect on emergency care”. Annals of Emergency Medicine, 68(1), 71.
Knapp, A. A., Lee, D. C., Borodovsky, J. T., Auty, S. G., Gabrielli, J., & Budney, A. J. (2019).” Emerging trends in cannabis administration among adolescent cannabis users.” Journal of Adolescent Health, 64(4), 487-493.
Mair, C., Freisthler, B., Ponicki, W. R., & Gaidus, A. (2015). “The impacts of marijuana dispensary density and neighborhood ecology on marijuana abuse and dependence.” Drug and Alcohol Dependence, 154, 111-116.
Mark, K., & Terplan, M. (2017). “Cannabis and pregnancy: maternal child health implications during a period of drug policy liberalization.” Preventive Medicine, 104, 46-49.
Mauro CM, Newswanger P, Santaella-Tenorio J, Mauro PM, Carliner H, Martins SS. (2019). “ Impact of medical marijuana laws on state-level marijuana use by age and gender, 2004-2013.” Prevention Sciences. 20: 205–214.
Midgette G, Davenport S, Caulkins JP, and B Kilmer, What America’s Users Spend on Illegal Drugs, 2006–2016. Santa Monica, CA: RAND Corporation, 2019. https://www.rand.org/pubs/research_reports/RR3140.html.
Miech, R., Patrick, M. E., O’malley, P. M., & Johnston, L. D. (2017). “What are kids vaping? Results from a national survey of US adolescents”. Tobacco Control, 26(4), 386-391.
National Academies of Sciences E, Medicine. (2017). The Health Effects of Cannabis and Cannabinoids: The Current State of Evidence and Recommendations for Research. Washington, DC: The National Academies Press.
National Institute on Drug Abuse (2019). Is Marijuana Use Safe While Pregnant or Breastfeeding? NIDA Policy Brief. Available at: https://www.drugabuse.gov/publications/marijuana-safe-to-use-while-pregnant-or-breastfeeding/marijuana-safe-to-use-while-pregnant-or-breastfeeding. Last accessed December 8, 2019.
Shen, J. J., Shan, G., Kim, P. C., Yoo, J. W., Dodge-Francis, C., & Lee, Y. J. (2019). “Trends and related factors of cannabis-associated emergency department visits in the United States: 2006–2014.” Journal of Addiction Medicine, 13(3), 193-200.
Shi, Y. (2017). “Medical marijuana policies and hospitalizations related to marijuana and opioid pain reliever.” Drug and Alcohol Dependence, 173, 144-150.
Smart, R., Caulkins, J. P., Kilmer, B., Davenport, S., and G Midgette (2017). Variation in cannabis potency and prices in a newly legal market: evidence from 30 million cannabis sales in Washington state. Addiction, 112(12), 2167-2177.
Smart R. and R.L. Pacula. (2019). “Early evidence of the impact of cannabis legalization on cannabis use, dependence and the use of other substances: A cautionary tale.” American Journal of Drug and Alcohol Abuse. Oct 13, 2019, 1-20.
Tormohlen, K. N., Brooks-Russell, A., Ma, M., Schneider, K. E., Levinson, A. H. and R.M. Johnson. (2019). Modes of marijuana consumption among Colorado high school students before and after the initiation of retail marijuana sales for adults. Journal of Studies on Alcohol and Drugs, 80(1), 46-55.
Volkow, N. D., Compton, W. M., & Wargo, E. M. (2017). The risks of marijuana use during pregnancy. JAMA, 317(2), 129-130.
Wang, G. S., Davies, S. D., Halmo, L. S., Sass, A., & Mistry, R. D. (2018). “Impact of marijuana legalization in Colorado on adolescent emergency and urgent care visits.” Journal of Adolescent Health, 63(2), 239-241.
Wang, G. S., Le Lait, M. C., Deakyne, S. J., Bronstein, A. C., Bajaj, L., & Roosevelt, G. (2016). Unintentional pediatric exposures to marijuana in Colorado, 2009-2015. JAMA Pediatrics, 170(9), e160971-e160971.
Wen H, Hockenberry JM, Cummings JR. (2015). “The effect of medical marijuana laws on adolescent and adult use of marijuana, alcohol, and other substances.” Journal of Health Economics. 42: 64–80.
Varner MW, Silver RM, Hogue CJR (2014). “Association between stillbirth and illicit drug use and smoking during pregnancy.” Obstetrics and Gynecology 123: 113-125.
Young-Wolff, K. C., Sarovar, V., Tucker, L. Y., Avalos, L. A et al. (2019). “Trends in marijuana use among pregnant women with and without nausea and vomiting in pregnancy, 2009–2016”. Drug and alcohol dependence, 196, 66-70.
Young-Wolff, K. C., Sarovar, V., Tucker, L. Y., Avalos, L. A., Conway, A., Armstrong, M. A., & Goler, N. (2018). Association of nausea and vomiting in pregnancy with prenatal marijuana use. JAMA Internal Medicine, 178(10), 1423-1424.
Zhu, H., & Wu, L. T. (2016). “Trends and correlates of cannabis-involved emergency department visits: 2004 to 2011.” Journal of Addiction Medicine, 10(6), 429.

You must be logged in to post a comment.