The Center for Medicare and Medicaid Innovation (CMMI) is tasked with testing new payment and delivery models and has undertaken a number of initiatives that bundle payments for episodes of care related to an acute hospitalization with care delivered after hospitalization.
Bundled payments have the potential to lower health care expenditures while preserving or even improving the quality of care received by beneficiaries by creating incentives around the delivery of a full episode of care.
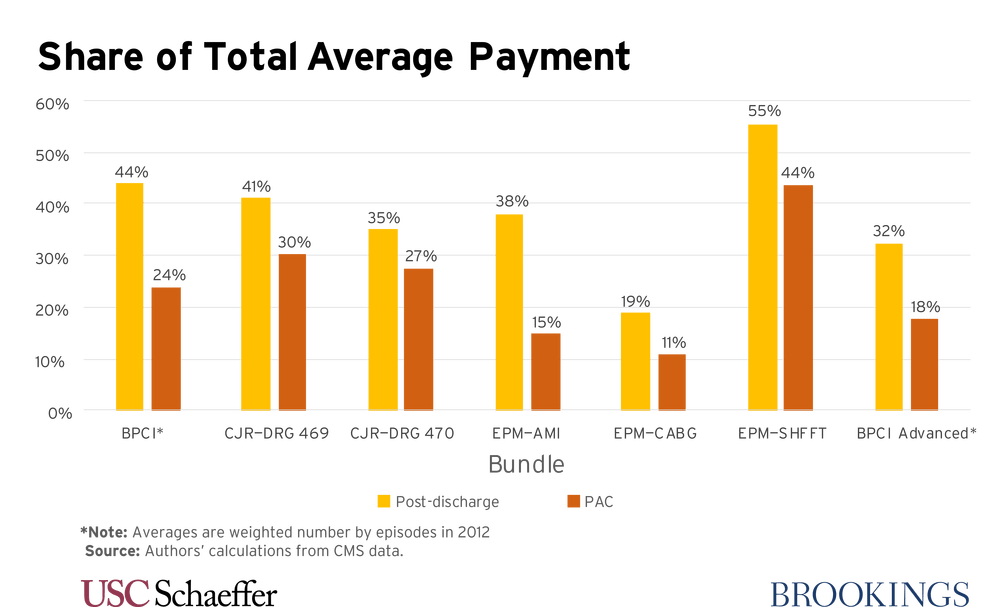
In fact, post-discharge and post-acute care (PAC) account for substantial fractions of spending in major CMMI bundled payment initiatives. In “Improving Bundled Payments in Medicare” (PDF), John A. Romley and Paul B. Ginsburg look at three ways to improve the effectiveness of these bundled payment systems.
Episodes based on an acute hospitalization should continue to play an important role in bundled payments
While a physician-oriented approach can have merit, there are important benefits to episodes that focus on hospitals. One is the magnitude of revenue flows into most hospitals, which can make sharing of financial risk of bundled payment with the Medicare program more feasible. In addition, episodes that incorporate outpatient care prior to any admission may need to be more customized, for example, with respect to the services that trigger an episode; such complexity would tend to increase the cost of developing a payment model.
Hospitals and physicians providing inpatient care may be better situated to collaborate with PAC providers, or otherwise exert some control over PAC. Episodes that typically involve more services post-discharge, and PAC in particular, may provide greater opportunities for improved performance. These episode types are likely to have relatively broad scope for coordinating and even redesigning the delivery of care across providers, with an emphasis on the utilization of a cost-efficient mix of services.
Decision makers should revisit mandatory participation by health care providers
The Comprehensive Care for Joint Replacement (CJR) Model is now mandatory in only 34 areas, and certain bundles in Bundled Payments for Care Improvement (BPCI) Advanced with substantial post-acute utilization saw little participation in BPCI (for example, cardiac defibrillator). Moreover, some and possibly many providers who would prove successful may elect not to participate, due to risk aversion and the frontloading of participation costs.
Voluntary participation can impair the ability to sustain and expand the benefits of payment and delivery reforms over time. Inability to understand fully the differences between participants and nonparticipants may preclude reliable inferences about the impact of these approaches from the experience of the volunteers.
By building the evidence base, a mandatory approach can help target models toward all of the providers that are able to achieve positive performance improvements and can also help to set target prices based on regional benchmarks.
Payments for hospitalization-based bundles should be risk-adjusted to a greater extent than has been the case
Risk adjustment becomes more critical when participation is mandatory and payment is set to a regional benchmark. Misalignments between provider payment and patient severity raise concerns as to whether providers have the resources needed to treat patients appropriately. Such misalignments can create incentives for providers to avoid beneficiaries who are sicker or costlier, or to skimp on their care.
Equity toward providers is important both for its own sake and for the political sustainability of a payment system. Risk adjustment can help to ensure that the desired incentives can be created while minimizing the risk borne by providers.
Conclusion
As the Center for Medicare and Medicaid Services develops new approaches to payment and delivery, the authors argue that hospitalization-based bundles, with appropriate adjustments to payment for patient severity, will continue to offer meaningful opportunities for improved performance within the health system, and encourage decision makers to make the most of these opportunities by adopting mandatory models that address the needs of both patients and providers.
The authors did not receive any financial support from any firm or person for this article or from any firm or person with a financial or political interest in this article. They are currently not an officer, director, or board member of any organization with an interest in this article.
Editor’s Note: This analysis is part of the USC-Brookings Schaeffer Initiative for Health Policy, which is a partnership between the Center for Health Policy at Brookings and the University of Southern California Schaeffer Center for Health Policy & Economics. The Initiative aims to inform the national health care debate with rigorous, evidence-based analysis leading to practical recommendations using the collaborative strengths of USC and Brookings.

You must be logged in to post a comment.