As dementia continues to impact millions of people worldwide, researchers and policymakers have urgently sought effective treatments to prevent and treat the disease. One promising area of research is the potential for existing medications for chronic conditions to reduce the risk of dementia or slow its onset. Researchers at the USC Schaeffer Center for Health Policy & Economics have been at the forefront of these investigations.
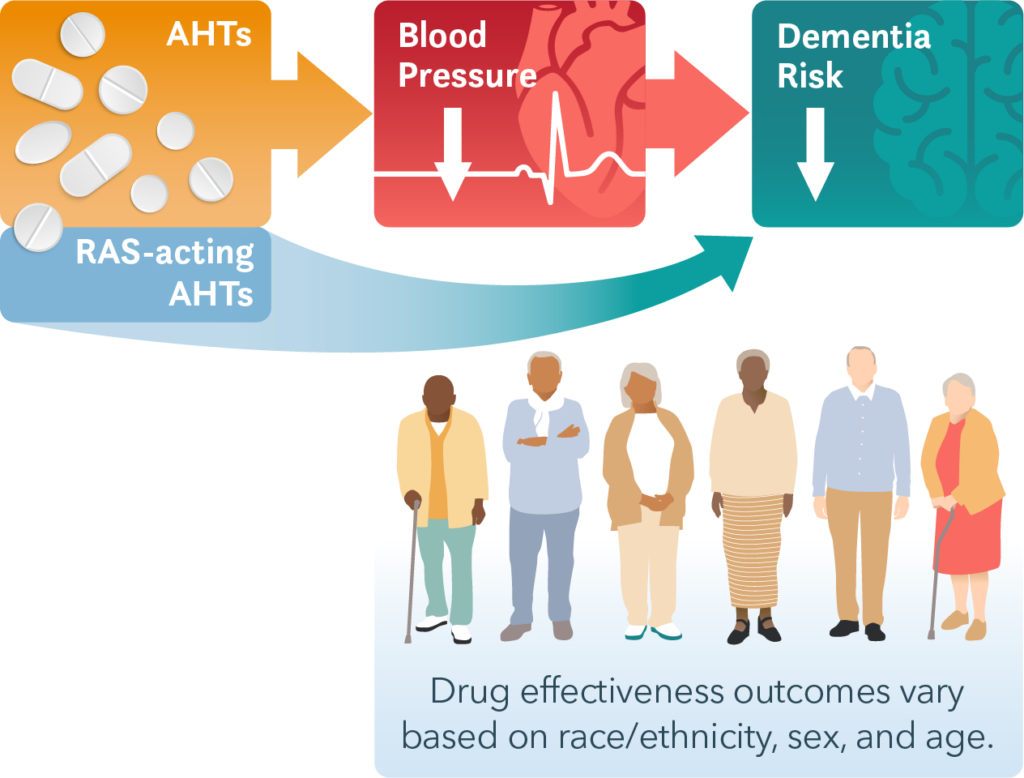
A growing body of research highlights existing blood pressure medications as one potential avenue for reducing dementia risk. Currently, nearly half of adults in the U.S. have high blood pressure, most of whom are prescribed blood pressure medication (called antihypertensives). Antihypertensives may reduce dementia risk directly by lowering blood pressure, a risk factor for cardiovascular disease, stroke and subsequent dementia. Some antihypertensives are hypothesized to impact Alzheimer’s disease pathology and provide further protection against this common form of dementia. Clinical trials have not yielded a definitive answer on the relationship between blood pressure medications and dementia. USC Schaeffer Center researchers have turned to real-world data to probe the relationship between antihypertensive use and dementia risk in the U.S. population and among minoritized populations who are at the highest risk of dementia.
Beyond blood pressure: antihypertensive drug class and dementia protection
A 2018 study led by Douglas Barthold, Geoffrey Joyce and Julie Zissimopoulos examined longitudinal data on the use of antihypertensive medications and new dementia diagnoses of millions of Medicare beneficiaries. With multiple classes of antihypertensive medications used to treat hypertension, the authors focused on distinguishing between them. The study reported that high blood pressure treatments that act on the renin-angiotensin hormone system (RAS) reduced the risk of dementia more than antihypertensives that do not act on this system. Importantly, the study provided insight into heterogeneity in effects for men and women and for different racial and ethnic persons. RAS-acting antihypertensives were associated with reduced risk of dementia in white men and white and Black women, but not in Hispanic men and women.
Many older individuals with hypertension also have other chronic conditions treated with pharmaceuticals. A second study conducted by the same team in 2020 found that the use of renin-angiotensin-related blood pressure drugs along with certain cholesterol-lowering drugs (pravastatin or rosuvastatin) was associated with reduced risk of developing dementia more than any other combination of cholesterol and antihypertensive medicines.
Two recent studies also reported heterogeneity in response to different classes of hypertensive medications. One, a randomized clinical trial from researchers at Uppsala University and the University of New South Wales, found considerable variation in individuals’ blood pressure response to four different classes of antihypertensives, including two that act on the renin-angiotensin system and two that do not. A recent study from researchers at the University of Washington reported results similar to early studies by the USC team. Study authors Zachary Marcum and colleagues found that antihypertensives that stimulate type 2 and 4 angiotensin II receptors were associated with lower risk of developing dementia compared to medications that inhibit those receptors.
The path forward
Antihypertensives may provide a low-cost and scalable opportunity to reduce dementia incidence worldwide. However, the considerable variation in individuals’ response to these medications points to potential benefits of personalized therapy. Real-world pragmatic trials may offer a strategy for measuring the complex relationships between medication class, sex, race and ethnicity for informing effective treatment and prevention strategies for dementia.
Affiliations
The USC Schaeffer Center for Health Policy and Economics researchers’ affiliations include: Schaeffer Center’s Aging and Cognition Research Program at the University of Southern California, USC’s Alzheimer’s Disease and Related Dementias Resource Center for Minority Aging Research (USC ADRD RCMAR) and the Center for Advancing Sociodemographic and Economic Study of Alzheimer’s Disease and Related Dementias (CeASES-ADRD).
Funding for this research was provided by RCMAR (P30AG043073) and CeASES ADRD (P30AG066589). Editorial support was provided by Rose Li and Associates.
Citations
Barthold, D., Joyce, G., Diaz Brinton, R., Wharton, W., Kehoe, P. G., & Zissimopoulos, J. (2020). Association of combination statin and antihypertensive therapy with reduced Alzheimer’s disease and related dementia risk. PloS one, 15(3), e0229541. https://doi.org/10.1371/journal.pone.0229541
Barthold, D., Joyce, G., Wharton, W., Kehoe, P., & Zissimopoulos, J. (2018). The association of multiple anti-hypertensive medication classes with Alzheimer’s disease incidence across sex, race, and ethnicity. PloS one, 13(11), e0206705. https://doi.org/10.1371/journal.pone.0206705
Marcum ZA, Gabriel N, Bress AP, Hernandez I. Association of New Use of Antihypertensives That Stimulate vs Inhibit Type 2 and 4 Angiotensin II Receptors With Dementia Among Medicare Beneficiaries. JAMA Netw Open. 2023;6(1):e2249370. doi:10.1001/jamanetworkopen.2022.49370
Sundström, J., Lind, L., Nowrouzi, S., Hagström, E., Held, C., Lytsy, P., … & Östlund, O. (2023). Heterogeneity in Blood Pressure Response to 4 Antihypertensive Drugs: A Randomized Clinical Trial. JAMA, 329(14), 1160-1169. https://doi.org/10.1001/jama.2023.3322
Thunell, J., Chen, Y., Joyce, G., Barthold, D., Shekelle, P. G., Brinton, R. D., & Zissimopoulos, J. (2021). Drug therapies for chronic conditions and risk of Alzheimer’s disease and related dementias: A scoping review. Alzheimer’s & Dementia, 17(1), 41-48. https://doi.org/10.1002/alz.12175
Sign up for Schaeffer Center news




You must be logged in to post a comment.