Even though racial disparities in mortality rates for older adults have narrowed, the gap between Black and White men in rural counties across the United States continues to widen. However, limited information regarding historical trends has made it hard to compare groups in urban societies with those in rural communities—or to understand the role played by race, gender and geography in these differences.
In a study published in August in JAMA Network Open, we used nationally representative data from 3,131 U.S. counties between 1968 and 2016 to help remedy this lack of knowledge. Our research examined three types of regions: urban counties, rural counties adjacent to an urban county and rural counties not adjacent to an urban county.
We found that rural and urban socioeconomic differences were associated with mortality rate disparities among both Black and White women. However, rural versus urban disparities in mortality rates among men remained significant—especially among Black men living in rural counties.
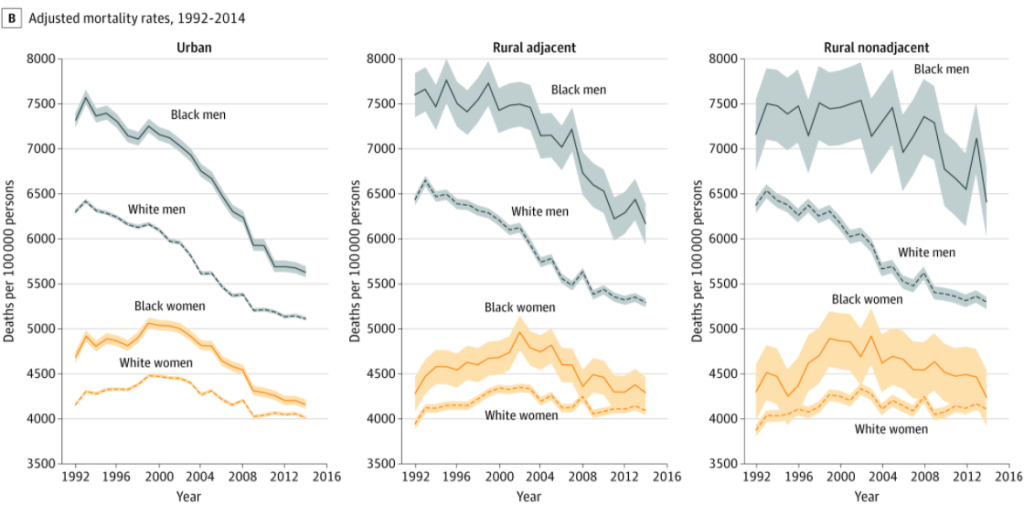
Notably, the current mortality rate of Black men in rural communities is similar to that of White men living in urban and rural areas in the mid-1980s. Understanding the intersectional factors associated with health disparities may help inform public health and clinical interventions.
New Insights into Rural Health Challenges
The increasing difficulty of accessing health care offers a major reason for this disparity. A long-lasting shortage of physicians in rural areas and closures of a disproportionate number of rural hospitals and nursing homes in the past 10 years have made health care both more expensive and geographically distant for many.
For example, after an older adult has a stroke, they may require post-acute inpatient rehabilitation care that lasts for months or years. Living in a rural area makes this care difficult to obtain. As African Americans face a higher risk of stroke—which itself is the product of structural racism, decreased access to rehabilitation services in rural areas puts them at higher risks of poor outcomes.
These findings are especially disturbing because the gap appears to be widening after accounting for socioeconomic characteristics. The evidence suggests that, 17 years after the Institute of Medicine’s landmark report Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care, our nation still neglects its recommendations for reducing this chasm in care.
We hope our findings will help policymakers understand mortality disparities and take measures to improve public health in rural regions, especially among older Black adults.
The full study can be found here.
Citation: Ferdows, N.B.; Aranda, M.P.; Baldwin, J.A.; Baghban Ferdows, S.; Ahluwalia, J.S.; Kumar, A. (2020). Assessment of Racial Disparities in Mortality Rates Among Older Adults Living in US Rural vs Urban Counties From 1968 to 2016. JAMA Network Open, 3(8), doi:10.1001/jamanetworkopen.2020.12241.
