What’s the latest in health policy research? The Essential Scan, produced by the Schaeffer Initiative for Innovation in Health Policy, aims to help keep you informed on the latest research and what it means for policymakers. To receive the Essential Scan in your inbox, sign up here.
Health checkups prompt increase in doctor visits but little change to health behaviors or outcomes
Toshiaki Iizuka, Katsuhiko Nishiyama, Brian Chen, and Karen Eggleston find that Japan’s mandatory annual health checkup programs increased the probability of visiting a physician from 10 to 15 percent, yet had little to no impact on health behaviors or outcomes. Following the argument that health checkups may raise awareness of and action to address health risks, the authors looked for aberrant health behavior and outcome trends among individuals identified with “borderline” risk for diabetes. The checkups somewhat increased the probability of walking or exercise among individuals with fasting blood glucose bordering high risk for the development of diabetes, but had little impact on smoking, drinking, or late-night eating habits. The authors observed little impact on intermediate- or longer-term health outcomes, such as fasting blood glucose levels or risk for stroke or congestive-heart failure. With diabetes as a focus of many U.S. population-health initiatives, these findings call into question patient responsiveness to preventive diabetes interventions, as well as their longer-term health and cost outcomes. Full article here.
Greater diffusion of low-quality drugs in U.S. compared to Australia, Canada, Switzerland, and United Kingdom
Margaret Kyle and Heidi Williams find greater diffusion of low-quality drugs relative to that of high-quality drugs in the U.S. as compared to Australia, Canada, Switzerland, and the United Kingdom. In their research, the authors used the French public health authority’s measure of drugs’ therapeutic value relative to existing treatments to differentiate high- and low-quality, looking solely at brand-name drugs launched on or after 2000 in both the U.S. and comparison countries. The authors compared the diffusions of low- and high-quality drugs in each country relative to each drug’s launch year in the respective country. These findings affirm previous assertions that the U.S. health care system is “uniquely inefficient,” and call for further investigation of and response to reasons for greater diffusion of low-quality drugs. Full article here.
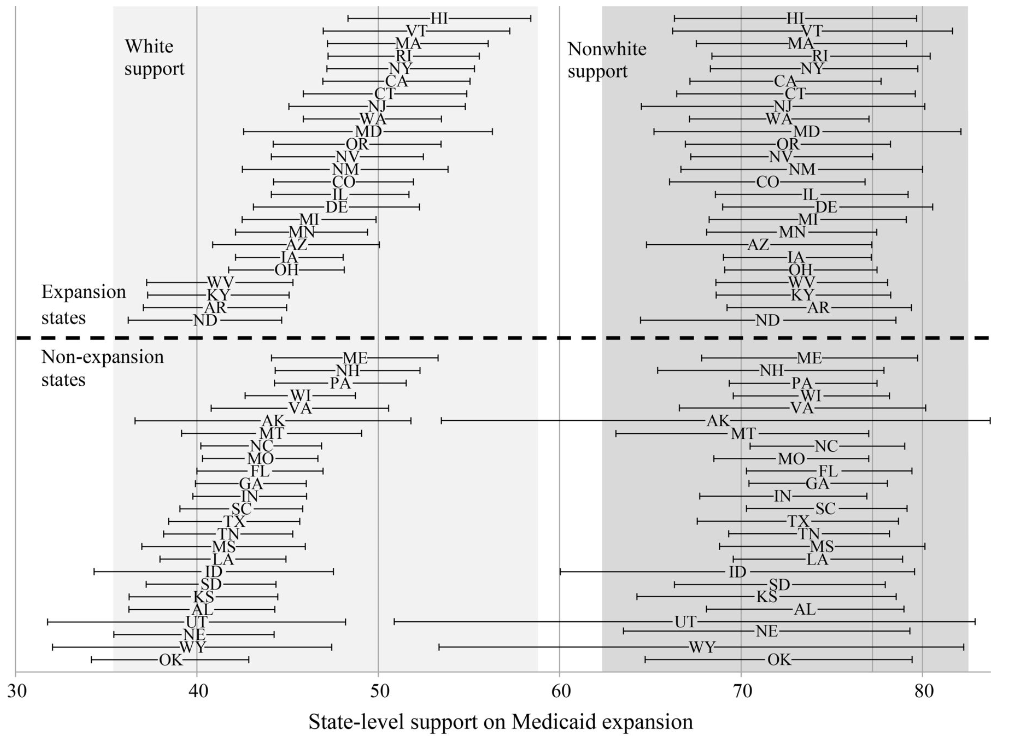
Public support associated with state Medicaid expansion, especially support among whites
Colleen M. Grogan and Sunggeun (Ethan) Park find that while overall state-level public support is positively correlated with expansion of Medicaid, support among whites is strongly associated with the state expanding Medicaid while nonwhite support played an insignificant role. Looking at state Medicaid expansion decisions relative to public support, the authors evaluate the applicability the authors’ “integrated racialized backlash theory,” which asserts that when white populations have low levels of support for a policy, an increasing share of a nonwhite population will increasingly be perceived as a threat and be resisted by whites. They find that the likelihood of a state expanding Medicaid decreases as the black share of the population increases in states with low-levels of white support for Medicaid expansion regardless of the levels of nonwhite support. In total, eight states’ actions on Medicaid expansion were out-of-step with public opinion, evenly divided among those that did not expand despite majority support and those that did despite majority opposition. These findings add concerning evidence on the role of public opinion and race in state-level policymaking. Full article here.
Major teaching hospitals’ mortality rates at 8.3 percent, compared to 9.5 in nonteaching hospitals
Laura G. Burke, Austin B. Frakt, Dhruv Khullar, and co-authors find that 30-day mortality rates for all hospitalizations were lower at major teaching hospitals than minor teaching or nonteaching hospitals after adjusting for patient and hospital characteristics (8.3, 9.2, and 9.5 percent, respectively). The authors found similar results when stratifying by size: the 30-day mortality rate was 8.1 percent among large teaching hospitals compared to 9.4 in large nonteaching hospitals, with similar patterns among small- and medium-sized hospitals. For this analysis, the authors used data on over 21 million hospitalizations of Medicare beneficiaries at over 4,400 U.S. hospitals. Further research is needed to understand the factors behind these disparate mortality findings among hospitals. Full article here.
Click here to receive The Essential Scan email.
Editor’s Note: The Essential Scan is produced by the Schaeffer Initiative for Innovation in Health Policy, a collaboration between the Center for Health Policy at the Brookings Institution and the USC Schaeffer Center for Health Policy & Economics. To receive the Essential Scan in your inbox, sign up here.