Surprise out-of-network bills arise when patients are treated by an out-of-network provider in a situation that cannot reasonably be avoided. Several recent studies highlight that surprise bills are a common occurrence. Most often, surprise bills arise in connection with services delivered by out-of-network emergency physicians or “ancillary” clinicians (e.g., radiology, anesthesiology, pathology, assistant or consulting surgeons, and hospitalists) at in-network facilities.
In all of these cases, the root cause of surprise billing is that patients lack a meaningful choice of providers. While patients do choose which hospital to go to for elective inpatient care and even frequently for emergency care, patients do not choose the emergency and ancillary clinicians that treat them, so the flow of patients that these specialists treat depends on the facility they practice at rather than which health plans they contract with. Emergency and ancillary clinicians, therefore, are guaranteed a flow of patients regardless of their network status, providing them a potentially lucrative out-of-network billing option that is unavailable in other specialties. The existence of this surprise billing option not only exposes patients to significant financial risk, but also drives up overall health care spending by allowing clinicians in these specialties to secure much higher payment rates.
One solution to most instances of surprise billing is to simply eliminate the possibility of being treated by an out-of-network emergency, ancillary, or similar clinician at an in-network facility. There are multiple ways to accomplish this, but one approach – sometimes called “network matching” or an “in-network guarantee” – would require these facility-based clinicians to contract with every health plan that the facility at which they practice accepts (or alternatively, choose to secure payment from the hospital rather than insurers). That requirement can be imposed either directly or, alternatively, indirectly by making joining an insurer’s network the only way clinicians can secure payment.
Network matching was one of three options included in a discussion draft released today by the chairman and ranking members of the Senate Health, Education, Labor and Pensions (HELP) Committee. House legislation introduced by Representative Lloyd Doggett and a proposal from hospital trade associations would effectively implement a similar approach. As we discuss below, network matching would be an effective solution to the most common instances of surprise billing and compares favorably to many of the most commonly discussed alternative approaches.
Why Surprise Billing Occurs
The existence of surprise billing represents a market failure that arises from two key features of this market. The first is that patients do not choose facility-based specialty clinicians, but these clinicians nevertheless contract independently with health plans. The second is that exposure to surprise out-of-network billing is not a salient enough consideration when consumers are choosing a hospital or insurer to give hospitals and insurers strong enough incentives to end the practice. Indeed, the idea that the anesthesiologist for your surgery might be out-of-network with your health plan when both the hospital and surgeon are in-network seems unlikely to cross most people’s minds (understandably so).
These features of the market leave many patients financially exposed when they seek care. They also drive up overall health care spending in two ways. First, the prices these physicians charge for services delivered out-of-network tend be extremely high. Second, and likely more important in practice, the existence of a lucrative out-of-network billing option allows these clinicians to demand very high payment rates even when they do agree to join insurers’ networks. Indeed, anesthesiologists, emergency medicine physicians, and radiologists are all paid average contracted rates at much higher multiples of the relevant Medicare rate than other specialties. Medicare rates are not a perfect measure of the relative cost of delivering different services, but this pattern is strongly consistent with the view that the threat of surprise billing patients gives these specialists substantial leverage.
How Network Matching Would Solve the Problem
Network matching would eliminate the possibility of surprise billing at in-network facilities by requiring facility-based emergency, ancillary, and similar clinicians to contract with all the same health plans as the facility as a condition of practicing at that facility. (We discuss how the Senate HELP network matching proposal would operationalize this requirement later in this post.)
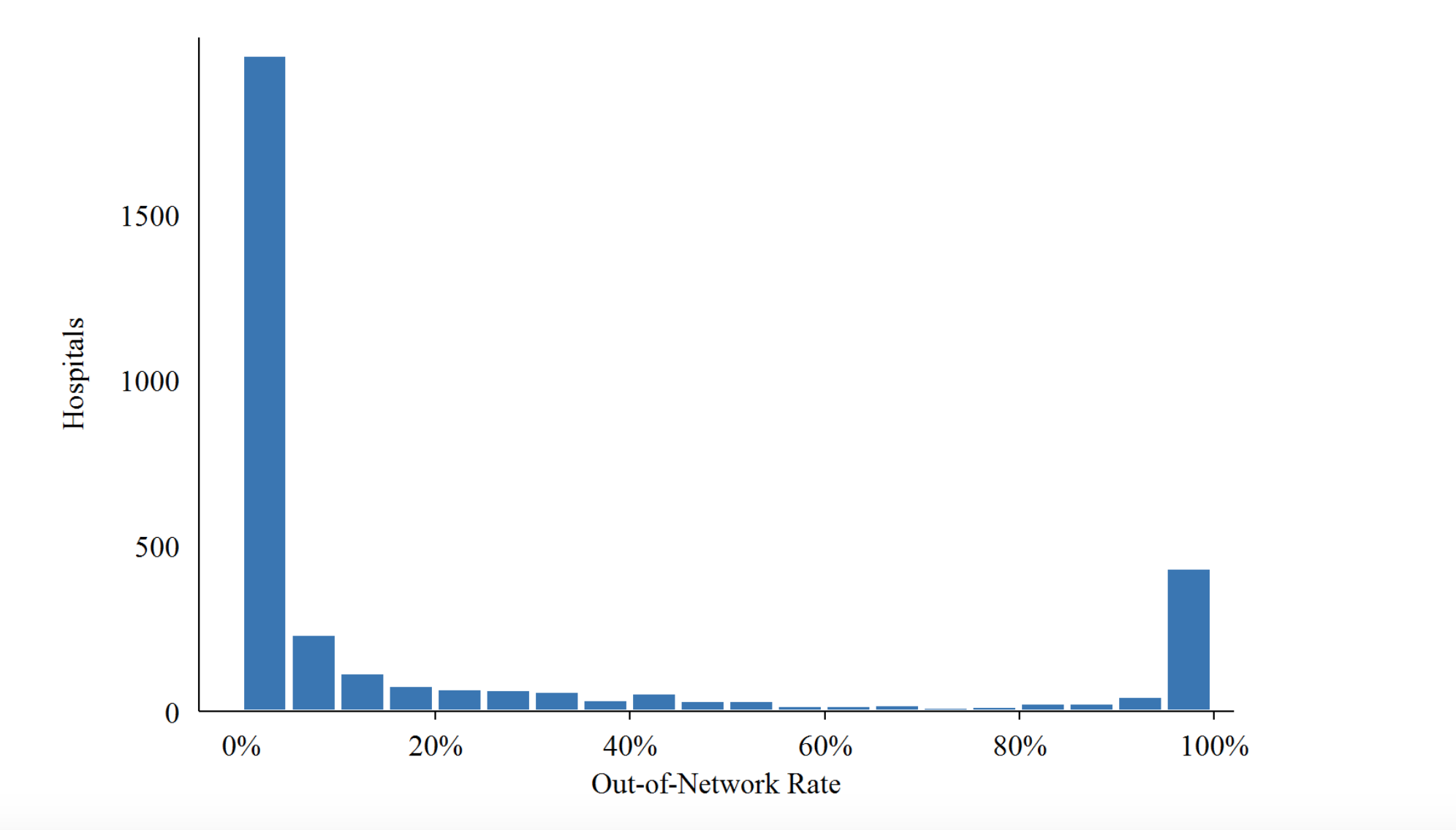
These clinicians already contract with and have a financial relationship with the facility at which they practice, and the facility is responsible for the flow of patients they treat, so it is natural to require concordant network contracting decisions. Moreover, many hospitals already effectively require this of their emergency and ancillary physicians. Indeed, using data from one large insurer, a paper from Zack Cooper, Fiona Scott Morton, and Nathan Shekita finds that 50 percent of hospitals have out-of-network billing rates in the emergency department below 2 percent, whereas 15 percent of hospitals have out-of-network billing rates of more than 80 percent.
Figure 2: The Distribution Of Hospital Out-Of-Network Billing Rates In 2015
Notes: The figure shows the distribution of emergency physician out-of-network billing rates across hospitals in 2015
Source: Cooper, Scott Morton, and Shekita 2019.
With such a policy in place, payment for these services would be negotiated among the insurer, hospital, and clinician. Some have suggested that this approach shifts too much leverage to insurers, who would know that these facility-based clinicians have to agree to contract terms in order to practice. However, this would not be a significant problem in practice because the hospital (or other facility) is contracting with both the insurer and clinicians, and the hospital needs to arrange for adequate payment to its clinicians in order to ensure adequate staffing. Thus, if insurers attempted to use this leverage to pay emergency and ancillary clinicians very low rates, the hospital would step in to insist that health plans offer reasonable rates as a condition of their contract with the hospital – or provide additional direct compensation to these clinicians and recover those costs from the payer.While the precise equilibrium payment rates for emergency and ancillary clinicians with this market failure removed are hard to predict, they would likely be notably lower than today’s contracted rates, which, as noted earlier, appear to be well above the levels that would prevail in a better-functioning market. Therefore, in addition to protecting patients from large unexpected bills, the network matching approach has the potential to generate significant premium savings for people enrolled in private insurance coverage, which could also generate federal budgetary savings by reducing the cost of the tax exclusion for employer-provided health insurance and the Affordable Care Act’s premium tax credit.
Comparing Network Matching to Other Approaches
Network matching is not the only approach to addressing surprise billing. One family of alternative approaches, which we have previously referred to as “billing regulation,” would limit the amounts that providers can collect for out-of-network services delivered at in-network facilities. That payment standard can either be specified directly in legislation or determined on case-by-case basis through arbitration. The recent draft legislation released by the Chairman and Ranking Member of the House Committee on Energy and Commerce took a billing regulation approach that specified a payment standard directly, while a recent discussion draft from a bipartisan group of senators took an arbitration approach. The Senate HELP discussion draft also presents two billing regulation options, one which directly specifies a payment standard and one which would implement an arbitration process.
In principle, billing regulation approaches can lead to outcomes that are very similar to those under a network matching approach—if the rate is set an appropriate level. In practice, however, the most prominent billing regulation proposals released to date have set the payment standard based on median in-network contracted rates. That approach largely locks in today’s inflated payment rates for these services, thereby forgoing much of the opportunity for surprise billing reform to reduce health care spending. Most such proposals have also specified that the in-network median would be computed on an insurer-specific basis, which creates the potential for gaming by both insurers and providers and can lock in an unlevel playing field across insurers. The Senate arbitration proposals have the same basic shortcomings, plus the arbitration process adds an additional layer of uncertainty and administrative cost. While these billing regulation proposals would likely still be an improvement on the status quo even with these shortcomings, a network matching approach could avoid these problems.
Another commonly discussed approach to addressing surprise billing is a “bundling” solution, in which facilities are effectively required to incorporate all emergency and ancillary clinicians services into the rates they negotiate with health plans; each of us have previously endorsed this approach. While the network matching approach is operationally distinct from “bundling,” we expect them to lead to very similar long-run outcomes since they both have the effect of requiring facilities and clinicians to negotiate jointly with insurers over the prices of the services delivered by emergency and ancillary clinicians. Because the network matching approach more closely resembles today’s system than the bundling approach, it would likely cause less immediate disruption and cause clinician payment rates to transition more slowly to the new equilibrium.
Separate proposals from Representative Lloyd Doggett and hospital trade groups would also effectively implement the network matching approach in most cases. Both proposals would prohibit out-of-network emergency and ancillary clinicians working at in-network facilities from billing patients for any amounts above their in-network cost-sharing requirement. Insurers would not be required to pay anything toward these surprise out-of-network bills, with the exception of emergency services, as discussed in greater detail below. As a result, these clinicians would effectively have to contract with the same health plans that the facility accepts in order to secure payment above the typically small patient in-network cost-sharing amounts. The one instance in which the Doggett and hospital trade group proposals could differ meaningfully from network matching is emergency services. If these statutory changes were made, it is unclear whether federal agencies would continue the administratively created “greatest of three” rule, which sets a minimum amount that insurers must pay for out-of-network emergency services. If the rule did remain in force, then, with respect to emergency services, these proposals would likely function more like a billing regulation approach with a payment standard tied to insurer-specific median in-network rates than a network matching approach.
What Services Should a Network Matching Requirement Apply to?
To be effective, a network matching requirement should apply to facility-based services where patients lack meaningful choice of providers, similar to where billing regulation approaches would apply. That includes: (1) out-of-network services provided by emergency and ancillary clinicians at an in-network facility; and (2) out-of-network laboratory or imaging services referred from an in-network facility.
For other out-of-network services delivered at an in-network facility, an exception could be allowed if the out-of-network clinician provides sufficient advance notice of their network status and estimated costs and obtains patient consent. This exception would allow, for example, a surgeon working at an in-network facility to treat patients on an out-of-network basis if both parties desire this arrangement.
How the Senate HELP Proposal Would Operationalize a Network Matching Approach
The key to operationalizing a network matching policy is to prohibit out-of-network emergency, ancillary, and similar clinicians practicing at an in-network facility from billing either patients or health plans (with the possible exception of the patient’s in-network cost sharing amounts). The Senate HELP discussion draft would do so in three steps. First, it would bar providers from billing patients directly for out-of-network services delivered at an in-network facility for amounts in excess of the in-network cost-sharing. Second, it would bar insurers from paying for any services delivered on an out-of-network basis at an in-network facility. Third, it would require all insurer-facility contracts to include a provision requiring the facility to ensure that all clinicians practicing at the facility join the insurer’s network. (This third requirement might not be strictly necessary once the other two changes are made.)
This approach would likely be largely successful in achieving network matching. However, providers and insurers could seek to skirt these requirements by setting up creative arrangements in which a facility was notionally out of network, but the facility tacitly agreed to accept a rate similar to the one it would have accepted in network and the insurer agreed to apply cost-sharing terms similar to in-network cost-sharing terms. The Senate HELP discussion draft includes some language that appears to be aimed at foreclosing this possibility, but it would be also worth considering additional safeguards. For example, a facility could be “deemed” as in-network for the purposes of these provisions if it treated a large enough fraction of an insurer’s enrollees in a given geographic area.
Notably, the network matching requirements in the current Senate HELP discussion draft applies more broadly to all out-of-network services at an in-network facility, not just out-of-network services delivered by emergency and ancillary clinicians. In revising the draft, consideration should be given to narrowing the requirement to exclude other categories of clinicians in cases where they meet notice and consent standards like the ones described above.
The Senate HELP discussion draft appears to envision allowing state surprise billing laws that meet certain standards to remain in force, rather than pre-empting those laws. However, the pre-emption language in the discussion draft has not been tailored to the three draft’s three distinct options for addressing surprise billing, so it is somewhat unclear how these exceptions would function in practice.
Cases Network Matching Cannot Address: Out-of-Network Facilities and Ambulances
The network matching approach solves most instances of surprise out-of-network billing, but inherently cannot address surprise bills from emergency and certain post-stabilization services at out-of-network facilities or out-of-network ambulances. These remaining surprise billing situations should be addressed by setting an explicit out-of-network payment standard, along the lines of billing regulation approaches discussed earlier.
The Senate HELP bill ties payment for emergency services delivered at an out-of-network facility to a health plan’s median in-network rate for similar services in a given geographic region. The draft instructs the Secretary of Health and Human Services to develop a more complete methodology and defaults to a market-wide median rate if a specific plan does not have sufficient in-network claims to reliably calculate a median.
Notably absent from the Senate HELP draft, in addition to every other Congressional bill this year, is any substantive attempt to address surprise out-of-network bills from ground or air ambulances.


You must be logged in to post a comment.